Comprehensive Analysis of Emerging Therapies and Innovations in Obesity Drugs and Delivery Platforms
ResearchAndMarket a leading market research provider, has released a comprehensive report titled “Growth Opportunities in Obesity Drugs and Delivery Platforms,” providing a thorough examination of the evolving landscape of obesity treatments and innovations in drug delivery.
Key Highlights:
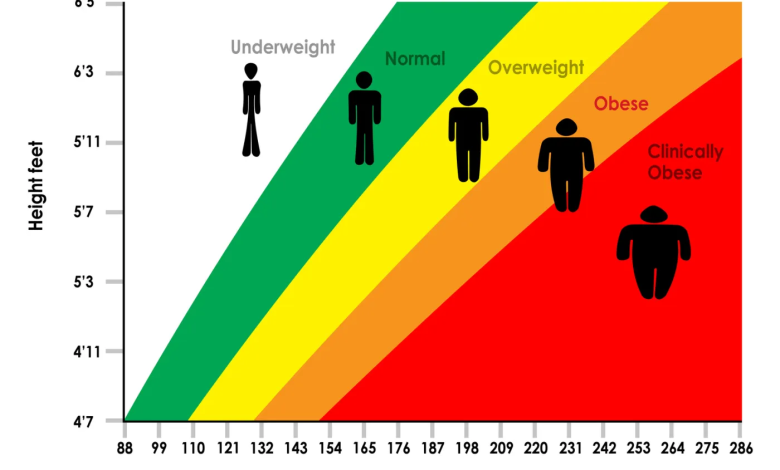
1. Paradigm Shift in Global Health Landscape:
• The report identifies a paradigm shift in the global health landscape, attributing it to the escalating burden of obesity. This shift is driving the development of novel medical interventions to address the critical challenges associated with obesity.
2. Exhaustive Analysis of Obesity Drugs and Delivery Platforms:
• Aiming to address the growing concern of obesity affecting both developed and developing nations, the report conducts an exhaustive analysis of emerging therapies and innovations in drug delivery platforms. It emphasizes the importance of lifestyle choices, a nutrient-rich diet, and collaboration with healthcare professionals in managing and mitigating obesity.
3. Focus on GLP-1-Based Treatments:
• The report highlights the increasing prominence of GLP-1-based treatments in the market. These treatments are gaining traction due to their efficacy and positive safety profiles in managing obesity and associated co-morbidities such as type 2 diabetes, cardiovascular diseases, and cancer.
4. User-Friendly Format:
• Structured in a user-friendly format, the publication provides insights into the dynamic funding landscape, clinical trial analysis, and a mechanistic dissection of promising anti-obesity drug candidates. It also offers an overview of advanced drug delivery technologies associated with obesity treatments.
5. Resource for Medical Professionals and Stakeholders:
• Positioned as a vital resource, the report is tailored to meet the needs of medical professionals, healthcare policymakers, and pharmaceutical companies involved in obesity treatment development. It aims to serve as a catalyst for innovation, policy revision, and strategic planning in the global fight against obesity and its associated health complications.
6. Encouraging Bold Strides in Medical Innovation:
• Acknowledging the global obesity crisis, the report advocates for bold strides in medical innovation and health policy. It encourages stakeholders to explore the comprehensive analysis, providing valuable insights into the future potential of obesity treatment modalities and drug delivery systems.
7. Accessible Insights for Healthcare Professionals and Decision-Makers:
• For those at the forefront of the obesity treatment landscape, the insights within this study are indispensable. Accessible to healthcare professionals, researchers, and decision-makers, the report aims to enhance understanding and address intricacies and opportunities within obesity pharmacotherapy and advanced delivery platforms.
Conclusion
This research publication stands as a compass, guiding the way forward in the battle against obesity. Stakeholders are invited to delve into this comprehensive analysis, leveraging the insights to navigate the evolving landscape of obesity treatment and contribute to impactful healthcare solutions.