Fentanyl: Uses, Side Effects, Abuse, Overdose
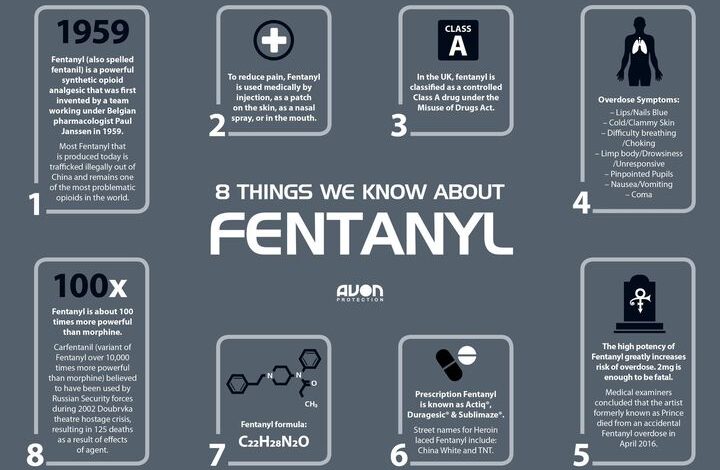
Fentanyl is a very powerful synthetic opioid analgesic that is similar to morphine but is 50 to 100 times more potent. It is a Schedule II prescription drug, and it is typically used to treat patients with severe pain or to manage pain after surgery. It is also sometimes used to treat patients with chronic pain who are physically tolerant to other opioids. In its prescription form, fentanyl is known by such names as Actiq®, Duragesic®, and Sublimaze®.
In general prescription, fentanyl is used to treat breakthrough pain (sudden episodes of pain that occur despite round the clock treatment with pain medication) in cancer patients at least 18 years of age (or at least 16 years of age if using Actiq brand lozenges) who are taking regularly scheduled doses of another narcotic (opiate) pain medication, and who are tolerant (used to the effects of the medication) to narcotic pain medications. Fentanyl is in a class of medications called narcotic (opiate) analgesics. It works by changing the way the brain and nervous system respond to pain.
Illegally synthesized fentanyl most often associated with recent overdoses is made in labs. This synthetic fentanyl is sold illegally as a powder, dropped onto blotter paper, put in eye droppers and nasal sprays, or made into pills that look like other prescription opioids.
Some drug dealers are mixing fentanyl with other drugs, such as heroin, cocaine, methamphetamine, and MDMA. This is because it takes very little to produce a high with fentanyl, making it a cheaper option. This is especially risky when people taking drugs don’t realize they might contain fentanyl as a cheap but dangerous additive. They might be taking stronger opioids than their bodies are used to and can be more likely to overdose.
How quickly does fentanyl work?
Fentanyl acts rapidly upon administration. Its onset of action depends on the route of administration:
1. Intravenous (IV) Injection: When fentanyl is administered intravenously, it usually takes effect within seconds to a couple of minutes. The rapid onset is due to the direct delivery of the drug into the bloodstream.
2. Transmucosal (Buccal, Sublingual, Intranasal): Fentanyl formulations designed for absorption through the mucous membranes (such as buccal, sublingual, or intranasal sprays) can also act relatively quickly. These routes allow fentanyl to bypass the digestive system and enter the bloodstream directly. The onset of action usually occurs within a few minutes.
It’s important to note that the potency and rapid onset of fentanyl increase its risk for overdose and respiratory depression. Fentanyl should only be used as prescribed by a healthcare professional and under proper medical supervision.
How should prescription fentanyl be used?
Fentanyl comes as a lozenge on a handle (Actiq), a sublingual (underneath the tongue) tablet (Abstral), a film (Onsolis), and a buccal (between the gum and cheek) tablet (Fentora) to dissolve in the mouth. Fentanyl is used as needed to treat breakthrough pain but not more often than four times a day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand.
Your doctor will probably start you on a low dose of fentanyl and gradually increase your dose until you find the dose that will relieve your breakthrough pain. If you still have pain 30 minutes after using fentanyl films (Onsolis), your doctor may tell you to use another pain medication to relieve that pain, and may increase your dose of fentanyl films (Onsolis) to treat your next episode of pain . Talk to your doctor about how well the medication is working and whether you are experiencing any side effects so that your doctor can decide whether your dose should be adjusted.
Do not use fentanyl more than four times a day. Call your doctor if you experience more than four episodes of breakthrough pain per day. Your doctor may need to adjust the dose of your other pain medication(s) to better control your pain.
Swallow the buccal tablet whole; do not split, chew, or crush. Also do not chew or bite the lozenge on a handle; only suck on this medication as directed.
Do not stop using fentanyl without talking to your doctor. Your doctor may decrease your dose gradually. If you suddenly stop using fentanyl, you may experience unpleasant withdrawal symptoms.
To use fentanyl lozenges (Actiq), follow these steps:
- Check the blister package and the handle of the lozenge to make sure the lozenge contains the dose of medication you have been prescribed.
- Use scissors to cut open the blister package and remove the lozenge. Do not open the blister package until you are ready to use the medication.
- Place the lozenge in your mouth, between your cheek and gum. Actively suck on the lozenge, but do not chew, crush, or bite it. Move the lozenge around in your mouth, from one side to the other, using the handle. Twirl the handle often.
- Do not eat or drink anything while the lozenge is in your mouth.
- Finish the lozenge in about 15 minutes.
- If you begin to feel dizzy, very sleepy, or nauseated before you have finished the lozenge, remove it from your mouth. Dispose of it immediately as described below or put it in the temporary storage bottle for later disposal.
- If you finish the entire lozenge, throw the handle away in a garbage can that is out of the reach of children. If you did not finish the entire lozenge, hold the handle under hot running water to dissolve all the medication, and then throw the handle away in a garbage can that is out of the reach of children and pets.
To use fentanyl buccal tablets (Fentora), follow these steps:
- Separate one blister unit from the blister card by tearing along the perforations. Peel back the foil to open the blister unit. Do not try to push the tablet through the foil. Do not open the blister unit until you are ready to use the tablet.
- Place the tablet in your mouth above one of your upper back teeth between your cheek and your gum.
- Leave the tablet in place until it dissolves completely. You may notice a gentle bubbling feeling between your cheek and gum as the tablet dissolves. It may take 14 to 25 minutes for the tablet to dissolve. Do not split, chew, bite, or suck the tablet.
- If any of the tablet is left in your mouth after 30 minutes, swallow it with a drink of water.
- If you begin to feel dizzy, very sleepy, or nauseated before the tablet dissolves, rinse your mouth with water and spit the remaining pieces of tablet into the sink or toilet. Flush the toilet or rinse the sink to wash away the tablet pieces.
To use fentanyl sublingual tablets (Abstral), follow these steps:
- Take a sip of water to moisten your mouth if it is dry. Spit out or swallow the water. Make sure your hands are dry before handling the tablet.
- Separate one blister unit from the blister card by tearing along the perforations. Peel back the foil to open the blister unit. Do not try to push the tablet through the foil. Do not open the blister unit until you are ready to use the tablet.
- Place the tablet under your tongue as far back as you can. If more than 1 tablet is needed for your dose, spread them around on the floor of your mouth under your tongue.
- Leave the tablet in place until it dissolves completely. Do not suck, chew, or swallow the tablet.
- Do not eat or drink anything until the tablet is completely dissolved and you no longer feel it in your mouth.
To use fentanyl films (Onsolis), follow these steps:
- Use scissors to cut along the arrows of the foil package to open it. Separate the layers of the foil package and remove the film. Do not open the foil package until you are ready to use the medication. Do not cut or tear the film.
- Use your tongue to wet the inside of your cheek, or if needed, rinse your mouth with water to wet the area where you will place the film.
- Hold the film on a clean, dry finger, with the pink side facing up. Place the film in your mouth, with the pink side against the inside of your moistened cheek. With your finger, press the film against your cheek for 5 seconds. Then remove your finger and the film will stick to the inside of your cheek. If more than one film is needed for your dose, do not put the films on top of each other. You may place the films on either side of your mouth.
- Leave the film in place until it dissolves completely. The film will release a minty flavor as it dissolves. It may take 15 to 30 minutes for the film to dissolve. Do not chew or swallow the film. Do not touch or move the film while it dissolves.
- You may drink liquids after 5 minutes, but do not eat anything until the film dissolves completely.
What side effects can this medication cause?
Fentanyl may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- drowsiness
- stomach pain
- gas
- heartburn
- weight loss
- difficulty urinating
- changes in vision
- anxiety
- depression
- unusual thinking
- unusual dreams
- difficulty falling asleep or staying asleep
- dry mouth
- sudden reddening of the face, neck, or upper chest
- uncontrollable shaking of a part of the body
- back pain
- chest pain
- pain, sores, or irritation in the mouth in the area where you placed the medication
- swelling of the hands, arms, feet, ankles, or lower legs
Some side effects can be serious. If you experience any of these symptoms, call your doctor immediately:
- changes in heartbeat
- agitation, hallucinations (seeing things or hearing voices that do not exist), fever, sweating, confusion, fast heartbeat, shivering, severe muscle stiffness or twitching, loss of coordination, nausea, vomiting, or diarrhea
- nausea, vomiting, loss of appetite, weakness, or dizziness
- inability to get or keep an erection
- irregular menstruation
- decreased sexual desire
- seizures
- hives
- rash
- itching
If you experience any of these symptoms, stop using fentanyl and call your doctor immediately or get emergency medical treatment:
- slow, shallow breathing
- decreased urge to breathe
- difficulty breathing or swallowing
- extreme drowsiness
- dizziness
- confusion
- fainting
Fentanyl may cause other side effects. Call your doctor if you have any unusual problems while using this medication.
If you experience a serious side effect, you or your doctor may send a report to the Food and Drug Administration’s (FDA) MedWatch Adverse Event Reporting program online or by phone (1-800-332-1088).
Fentanyl Safety Information
Fentanyl may be habit forming, especially with prolonged use. Use fentanyl exactly as directed. Do not use a larger dose of fentanyl, use the medication more often, or use it for a longer period of time than prescribed by your doctor. While using fentanyl, discuss with your healthcare provider your pain treatment goals, length of treatment, and other ways to manage your pain. Tell your doctor if you or anyone in your family drinks or has ever drunk large amounts of alcohol, uses or has ever used street drugs, or has overused prescription medications, or has had an overdose, or if you have or have ever had depression or another mental illness. There is a greater risk that you will overuse fentanyl if you have or have ever had any of these conditions. Talk to your health care provider immediately and ask for guidance if you think that you have an opioid addiction or call the U.S. Substance Abuse and Mental Health Services Administration (SAMHSA) National Helpline at 1-800-662-HELP.
Fentanyl should only be prescribed by doctors who are experienced in treating pain in cancer patients. It should be used only to treat breakthrough cancer pain (sudden episodes of pain that occur despite around-the-clock treatment with pain medication) in cancer patients at least 18 years of age (or at least 16 years of age if using Actiq brand lozenges) who are taking regularly scheduled doses of another narcotic (opiate) pain medication, and who are tolerant (used to the effects of the medication) to narcotic pain medications. This medication should not be used to treat pain other than chronic cancer pain, especially short-term pain such as migraines or other headaches, pain from an injury, or pain after a medical or dental procedure. Fentanyl may cause serious breathing problems or death if it is used by people who are not being treated with other narcotic medications or who are not tolerant to narcotic medications.
Fentanyl may cause serious harm or death if used accidentally by a child or by an adult who has not been prescribed the medication. Even partially used fentanyl may contain enough medication to cause serious harm or death to children or other adults. Keep fentanyl out of reach of children, and if you are using the lozenges, ask your doctor how to obtain a kit from the manufacturer containing child safety locks and other supplies to prevent children from getting the medication. Dispose partially used lozenges according to the manufacturer’s directions immediately after you remove them from your mouth. If fentanyl is used by a child or an adult who has not been prescribed the medication, try to remove the medication from the person’s mouth and get emergency medical help.
Fentanyl should be used along with your other pain medication(s). Do not stop taking your other pain medication(s) when you begin your treatment with fentanyl. If you stop taking your other pain medication(s) you will need to stop using fentanyl.
If you still have pain after using one lozenge or tablet, your doctor may tell you to use a second lozenge or tablet. You may use the second lozenge (Actiq) 15 minutes after you finish the first lozenge, or use the second tablet (Abstral, Fentora) 30 minutes after you started using the first tablet. Do not use a second lozenge or tablet to treat the same episode of pain unless your doctor tells you that you should. If you are using fentanyl film (Onsolis), you should not use a second dose to treat the same episode of pain. After you treat an episode of pain using 1 or 2 doses of fentanyl as directed, you must wait at least 2 hours after using fentanyl (Abstral or Onsolis) or 4 hours after using fentanyl (Actiq or Fentora) before treating another episode of breakthrough cancer pain.
Taking certain medications with fentanyl may increase the risk that you will develop serious or life-threatening breathing problems, sedation, or coma. Tell your doctor if you are taking any of the following medications: amiodarone (Nexterone, Pacerone); certain antibiotics such as clarithromycin (Biaxin, in PrevPac), erythromycin (Erythocin), telithromycin (Ketek), and troleandomycin (TAO) (not available in the US); certain antifungals such as fluconazole (Diflucan), itraconazole (Onmel, Sporanox), and ketoconazole (Nizoral); aprepitant (Emend); benzodiazepines such as alprazolam (Xanax), chlordiazepoxide (Librium), clonazepam (Klonopin), diazepam (Diastat, Valium), estazolam, flurazepam, lorazepam (Ativan), oxazepam, temazepam (Restoril), and triazolam (Halcion); cimetidine (Tagamet); diltiazem (Cardizem, Taztia, Tiazac, others); certain medications for human immunodeficiency virus (HIV) such as amprenavir (Agenerase), fosamprenavir (Lexiva), indinavir (Crixivan), nelfinavir (Viracept), ritonavir (Norvir, in Kaletra), and saquinavir (Invirase); medications for mental illness and nausea; muscle relaxants; nefazodone; sedatives; sleeping pills; tranquilizers; or verapamil (Calan, Covera, Verelan). Your doctor may need to change the dosages of your medications and will monitor you carefully. If you use fentanyl with any of these medications and you develop any of the following symptoms, call your doctor immediately or seek emergency medical care: unusual dizziness, lightheadedness, extreme sleepiness, slowed or difficult breathing, or unresponsiveness. Be sure that your caregiver or family members know which symptoms may be serious so they can call the doctor or emergency medical care if you are unable to seek treatment on your own.
Fentanyl comes as four different transmucosal products and several other types of products. The medication in each product is absorbed differently by the body, so one product cannot be substituted for any other fentanyl product. If you are switching from one product to another, your doctor will prescribe a dose that is best for you.
A program has been set up for each fentanyl product to decrease the risk of using the medication. Your doctor will need to enroll in the program in order to prescribe fentanyl and you will need to have your prescription filled at a pharmacy that is enrolled in the program. As part of the program, your doctor will talk with you about the risks and benefits of using fentanyl and about how to safely use, store, and dispose of the medication. After you talk with your doctor, you will sign a form acknowledging that you understand the risks of using fentanyl and that you will follow your doctor’s instructions to use the medication safely. Your doctor will give you more information about the program and how to get your medication and will answer any questions you have about the program and your treatment with fentanyl.
Your doctor or pharmacist will give you the manufacturer’s patient information sheet (Medication Guide) when you begin treatment with fentanyl and each time you get more medication. Read the information carefully and ask your doctor or pharmacist if you have any questions. You can also visit the Food and Drug Administration (FDA) website
How to overcome fentanyl abuse
Overcoming fentanyl abuse can be a challenging process, but with the right support and treatment, recovery is possible. Here are some steps that can help:
1. Recognize the problem: Acknowledge that you have a problem with fentanyl abuse. Denial can hinder your progress, so it’s crucial to honestly assess your situation and understand the negative impact it has on your life.
2. Seek professional help: Consult a healthcare professional or addiction specialist who can guide you through the recovery process. They can provide medical assessment, create a personalized treatment plan, and recommend appropriate interventions.
3. Detoxification: Since fentanyl is a highly potent opioid, detoxification should be conducted under medical supervision. This allows for the safe withdrawal from the drug while managing withdrawal symptoms and potential complications.
4. Inpatient or outpatient treatment: Depending on the severity of the addiction, you may choose between inpatient or outpatient treatment programs. Inpatient programs offer a structured environment with 24/7 medical care and counseling, while outpatient programs provide treatment on a scheduled basis while allowing you to live at home.
5. Behavioral therapies: Engage in behavioral therapies such as cognitive-behavioral therapy (CBT) or contingency management. These therapies aim to identify triggers and develop coping mechanisms, manage cravings, and modify unhealthy thought patterns and behaviors associated with fentanyl abuse.
6. Support groups: Join support groups such as Narcotics Anonymous (NA) or other addiction recovery programs. These groups provide a supportive community of individuals who have faced similar challenges and can offer guidance, encouragement, and accountability.
7. Develop a relapse prevention plan: Work with your healthcare professional to develop a relapse prevention plan that includes strategies for managing triggers, stress, and cravings. Identify healthy coping mechanisms and establish a support network of family, friends, or sponsors who can provide assistance during challenging times.
8. Address co-occurring conditions: If you have underlying mental health issues such as depression or anxiety, it’s important to address them alongside your substance abuse treatment. Treating co-occurring conditions improves the chances of successful recovery.
Remember, overcoming fentanyl abuse is a journey that requires commitment, patience, and support. It’s important to surround yourself with a strong support system and access professional help to increase your chances of a successful recovery.