Suboxone Strips: Uses, Dosage, Benefits, Side Effects, Interactions
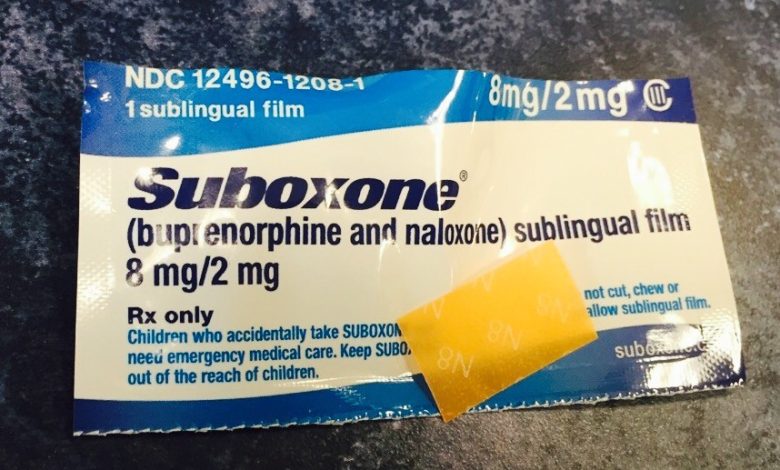
Suboxone strips, also known as Suboxone film, are a specific formulation of the medication Suboxone that comes in a strip format. These strips are designed to be placed under the tongue, where they dissolve and deliver the medication into the bloodstream.
Suboxone strips are used as part of medication-assisted treatment (MAT) for opioid dependence and addiction. They contain a combination of buprenorphine and naloxone. Here’s a breakdown of the components:
1. Buprenorphine: It is a partial opioid agonist, which means it binds to the opioid receptors in the brain, but its effects are milder compared to full agonists like heroin or oxycodone. Buprenorphine helps to reduce cravings and withdrawal symptoms associated with opioid addiction.
2. Naloxone: It is an opioid antagonist that blocks the effects of other opioids. Naloxone is included in Suboxone to deter misuse and abuse. When taken sublingually as directed, the naloxone has minimal effect. However, if someone were to attempt to misuse Suboxone by crushing and injecting it, the naloxone can precipitate withdrawal symptoms.
The strips are typically thin and dissolvable, making them easy to administer and ensuring the proper absorption of the medication. They come in various strengths, including 2 mg, 4 mg, 8 mg, and higher doses, allowing for flexibility in dosing based on individual needs and treatment plans.
Suboxone strips are usually prescribed as part of a comprehensive treatment program that includes counseling, therapy, and support services. They are intended for long-term use to help individuals with opioid addiction stabilize their lives and reduce the risk of relapse.
It’s important to note that Suboxone should only be used under the guidance and prescription of a healthcare professional who specializes in addiction medicine. Deviating from the prescribed dosage or using Suboxone without medical supervision can have serious consequences and may lead to adverse effects or complications.
Dosage of Suboxone strips
The dosage of Suboxone strips, like any medication, is determined by a healthcare professional based on individual needs and response to treatment. The appropriate dosage can vary depending on factors such as the severity of opioid dependence, previous treatment history, and other individual considerations.
Suboxone strips come in various strengths, including 2 mg, 4 mg, 8 mg, and higher doses. The goal of Suboxone treatment is to find the lowest effective dose that helps manage cravings and withdrawal symptoms while minimizing the risk of side effects.
The initial dosage and subsequent adjustments are typically made by a healthcare professional with expertise in addiction medicine. They will carefully evaluate the individual’s condition and response to treatment to determine the appropriate starting dose.
In general, the following dosing guidelines may be considered:
1. Induction phase: The initial dose is typically started low and gradually increased until the individual achieves stability. It is common to begin with a lower dose, such as 2 mg or 4 mg, and assess the response over several days. The dosage can be adjusted accordingly to find the optimal dose for the individual.
2. Maintenance phase: Once stability is achieved, the dosage is generally maintained for an extended period, which may vary depending on the individual’s treatment plan. The maintenance dose is aimed at preventing withdrawal symptoms and reducing cravings. It is usually within the range of 4 mg to 24 mg per day, depending on individual needs.
It’s important to follow the prescribed dosage and administration instructions provided by the healthcare professional. Regular follow-up appointments will be scheduled to monitor progress, adjust the dosage if needed, and provide ongoing support throughout the treatment process.
It’s worth emphasizing that the dosage of Suboxone should only be determined and modified by a qualified healthcare professional. Self-adjusting the dosage or using Suboxone without medical supervision can be dangerous and may lead to adverse effects or complications. It’s essential to maintain open and honest communication with the healthcare provider regarding any concerns, side effects, or changes in the individual’s condition.
Benefits of Suboxone strips
Suboxone strips offer several benefits as a medication-assisted treatment (MAT) option for individuals with opioid dependence or addiction. Here are some of the key benefits:
1. Reduced withdrawal symptoms: Suboxone contains buprenorphine, a partial opioid agonist that helps to alleviate withdrawal symptoms commonly experienced during opioid detoxification. By binding to the opioid receptors in the brain, buprenorphine can help stabilize the individual and reduce the discomfort associated with withdrawal.
2. Craving reduction: Suboxone’s buprenorphine component also helps to suppress cravings for opioids. By occupying the opioid receptors in the brain, buprenorphine can help reduce the desire to use opioids, making it easier for individuals to abstain from illicit drugs.
3. Naloxone’s protective effect: Suboxone strips contain naloxone, an opioid antagonist. While naloxone has a minimal effect when taken sublingually as directed, it serves as an important safeguard against misuse. If someone attempts to misuse Suboxone by crushing and injecting it, the naloxone can induce withdrawal symptoms, acting as a deterrent against misuse and reducing the risk of abuse.
4. Easy administration: Suboxone strips are designed to be placed under the tongue, where they dissolve and are absorbed into the bloodstream. This sublingual administration route is convenient and easy to follow, making it accessible for individuals undergoing treatment.
5. Long-lasting effects: Suboxone has a long half-life, meaning it remains active in the body for an extended period. This allows for once-daily or less frequent dosing, providing stable medication levels and reducing the need for frequent administration.
6. Comprehensive treatment approach: Suboxone is typically used as part of a comprehensive treatment program that includes counseling, therapy, and support services. This holistic approach addresses not only the physical aspects of addiction but also the psychological and social factors contributing to it, improving the chances of long-term recovery.
7. Decreased risk of overdose: Suboxone, when taken as prescribed, carries a lower risk of overdose compared to full opioid agonists. The presence of naloxone in Suboxone further reduces the risk of respiratory depression and overdose.
It’s important to note that the benefits of Suboxone strips should be weighed against individual considerations and potential side effects. The decision to use Suboxone as part of MAT should be made in consultation with a qualified healthcare professional who specializes in addiction medicine. They can evaluate the individual’s specific needs, medical history, and treatment goals to determine the most appropriate approach to recovery.
Suboxone Strips Side Effects
Like any medication, Suboxone strips can cause side effects. It’s important to note that not everyone will experience these side effects, and their severity can vary from person to person. Common side effects associated with Suboxone strips may include:
1. Nausea and vomiting: Gastrointestinal disturbances such as nausea and vomiting are among the most commonly reported side effects of Suboxone. Taking the medication with food or adjusting the timing of administration may help reduce these symptoms.
2. Headache: Some individuals may experience headaches while taking Suboxone. Staying hydrated, managing stress, and using over-the-counter pain relievers (under medical supervision) can often help alleviate these symptoms.
3. Constipation: Opioid medications, including Suboxone, can slow down bowel movements and lead to constipation. Adequate fluid intake, a high-fiber diet, and the use of stool softeners or laxatives (under medical guidance) can help manage this side effect.
4. Insomnia or sleep disturbances: Suboxone can affect sleep patterns, leading to difficulty falling asleep or staying asleep. It is important to discuss any sleep disturbances with the healthcare provider, as they may recommend strategies or adjustments to help improve sleep quality.
5. Sweating: Excessive sweating or changes in sweating patterns can occur as a side effect of Suboxone. Staying well-hydrated and avoiding excessive heat or strenuous activity can help manage this symptom.
6. Dizziness or lightheadedness: Some individuals may experience feelings of dizziness or lightheadedness while taking Suboxone. It is important to avoid activities that require alertness until the body adjusts to the medication.
7. Allergic reactions: Although rare, some individuals may have an allergic reaction to Suboxone. Symptoms may include rash, itching, swelling, severe dizziness, or difficulty breathing. Immediate medical attention should be sought if any signs of an allergic reaction occur.
It’s important to promptly report any side effects to a healthcare professional. They can evaluate the severity and provide guidance on managing side effects or adjusting the medication dosage if necessary. It’s worth noting that the benefits of Suboxone in the treatment of opioid dependence generally outweigh the potential side effects. Healthcare professionals carefully consider the risks and benefits when prescribing Suboxone and work closely with individuals to monitor their response to the medication.
This is not an exhaustive list of side effects, and other rare or less common side effects may occur. It’s crucial to consult a healthcare professional for comprehensive information about potential side effects specific to your situation.
Suboxone Strips Interactions
Suboxone strips can interact with certain substances, medications, or medical conditions. It is important to disclose all medications, supplements, and medical conditions to your healthcare provider before starting Suboxone treatment. Here are some notable interactions:
1. Opioid medications: Suboxone contains buprenorphine, which is a partial opioid agonist. Concurrent use of other opioid medications, such as painkillers or certain cough suppressants, can increase the risk of respiratory depression and other opioid-related side effects. It’s crucial to inform your healthcare provider about any other opioids you are taking.
2. Benzodiazepines and sedatives: Combining Suboxone with benzodiazepines, sedatives, or tranquilizers can lead to increased sedation and respiratory depression. These medications include drugs like alprazolam (Xanax), diazepam (Valium), and zolpidem (Ambien). Extreme caution is needed when using these medications together, and close monitoring by a healthcare professional is essential.
3. Central nervous system (CNS) depressants: Suboxone can enhance the effects of other CNS depressants, such as alcohol, barbiturates, muscle relaxants, and certain antihistamines. This combination can lead to increased sedation, respiratory depression, and impaired cognitive function. Avoid or use these substances with caution, and consult your healthcare provider for guidance.
4. Monoamine oxidase inhibitors (MAOIs): MAOIs are a class of antidepressant medications that can interact with Suboxone and increase the risk of serotonin syndrome. Serotonin syndrome is a potentially life-threatening condition characterized by agitation, confusion, rapid heart rate, high blood pressure, and tremors. Inform your healthcare provider if you are taking or have recently taken MAOIs.
5. Hepatitis C medications: Some medications used to treat hepatitis C, such as certain protease inhibitors and non-nucleoside reverse transcriptase inhibitors, may interact with Suboxone. These interactions can affect the metabolism and clearance of Suboxone, potentially altering its effectiveness or increasing the risk of side effects. Close monitoring is needed when Suboxone is used alongside hepatitis C medications.
6. Medical conditions: Inform your healthcare provider about any medical conditions you have, especially liver disease, kidney disease, respiratory disorders, or a history of seizures. These conditions may require specific monitoring or dosage adjustments when using Suboxone.
This list is not exhaustive, and other medications or substances may interact with Suboxone. It is essential to consult with a healthcare professional or pharmacist to get comprehensive information about potential interactions specific to your situation. Never start or stop any medication or substance without medical guidance while taking Suboxone.





