List Of Cyclobenzaprine Interactions You Should Know
Drug interactions involve combinations of a medication with other substances that alter the medication’s effect on the body. If you use multiple medications, have certain health conditions, or see more than one doctor, you should be especially mindful of your medications. You also need to make sure that each of your doctors know all of the drugs, herbs, supplements, and vitamins you’re using.
This is because drug interactions may make your drug less effective, cause unexpected side effects, or increase the action of a particular drug. Some drug interactions can even be harmful to you. Reading the label every time you use a nonprescription or prescription drug and taking the time to learn about drug interactions may be critical to your health. You can reduce the risk of potentially harmful drug interactions and side effects with a little bit of knowledge and common sense. Drug interactions fall into three broad categories:
- Drug-drug interactions occur when two or more drugs react with each other. This drug-drug interaction may cause you to experience an unexpected side effect. For example, mixing a drug you take to help you sleep (a sedative) and a drug you take for allergies (an antihistamine) can slow your reactions and make driving a car or operating machinery dangerous.
- Drug-food/beverage interactions result from drugs reacting with foods or beverages. For example, mixing alcohol with some drugs may cause you to feel tired or slow your reactions.
- Drug-condition interactions may occur when an existing medical condition makes certain drugs potentially harmful. For example, if you have high blood pressure you could experience an unwanted reaction if you take a nasal decongestant.
What is cyclobenzaprine?
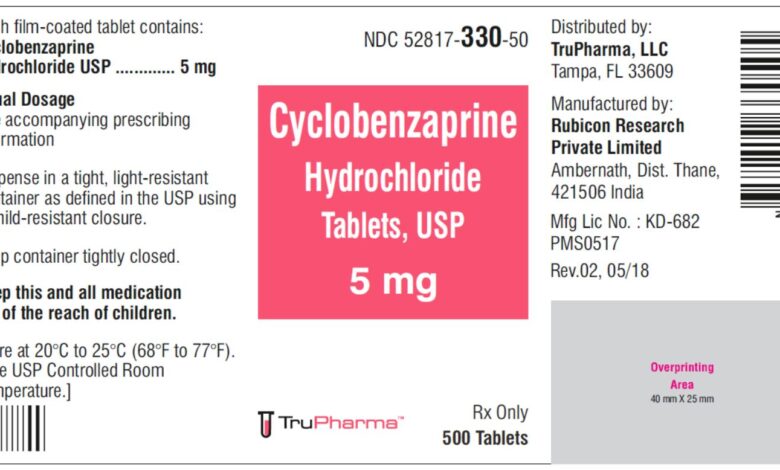
Cyclobenzaprine is in a class of medications called skeletal muscle relaxants. It is a centrally-acting muscle relaxant that works by acting in the brain and nervous system to allow the muscles to relax.
This drug was first synthesized in 1961 and became available for human use in 1977. It was initially studied for use as antidepressant given its structural similarity to tricyclic antidepressants – it differs from Amitriptyline by only a single double bond.
Cyclobenzaprine is used with rest, physical therapy, and other measures to relax muscles and relieve pain and discomfort caused by strains, sprains, and other muscle injuries.
List Of Cyclobenzaprine Interactions
There may be an interaction between cyclobenzaprine and any of the following:
• abiraterone acetate
• aclidinium
• amlodipine
• amphetamines (e.g., dextroamphetamine, lisdexamphetamine)
• antihistamines (e.g,. cetirizine, doxylamine, diphenhydramine, hydroxyzine, loratadine)
• antipsychotics (e.g., chlorpromazine, clozapine, haloperidol, olanzapine, quetiapine, risperidone)
• atropine
• azelastine
• belladonna
• benzodiazepines (e.g., alprazolam, diazepam, lorazepam)
• benztropine
• botulinum toxin
• brimonidine
• bromocriptine
• buspirone
• cannabis
• certain quinolone antibiotics (e.g., ciprofloxacin, norfloxacin, ofloxacin)
• cimetidine
• darifenacin
• deferasirox
• dextromethorphan
• disopyramide
• domperidone
• entacapone
• ergot alkaloids (e.g., ergotamine, dihydroergotamine)
• ethinyl estradiol
• fesoterodine
• flavoxate
• gemfibrozil
• glucagon
• glycopyrrolate
• ipratropium
• kava kava
• ketoconazole
• lithium
• magnesium sulphate
• methylene blue
• methoxsalen
• metoclopramide
• metyrosine
• mexiletine
• mianserin
• minocycline
• mirabegron
• mirtazapine
• monoamine oxidase inhibitors (MAOIs; e.g., moclobemide, rasagiline, selegiline, tranylcypromine)
• narcotic pain relievers (e.g., codeine, fentanyl, morphine, oxycodone)
• nabilone
• nifedipine
• orphenadrine
• oxybutynin
• peginterferon alfa-2b
• potassium chloride
• pramipexole
• pramlintide
• primaquine
• rivastigmine
• ropinirole
• rotigotine
• St. John’s wort
• scopolamine
• seizure medications (e.g., carbamazepine, clobazam, levetiracetam, phenobarbital, phenytoin, primidone, topiramate, valproic acid)
• serotonin antagonists (anti-emetic medications; e.g., granisetron, ondansetron)
• serotonin/norepinephrine reuptake inhibitors (SNRIs; e.g., desvenlafaxine, duloxetine, venlafaxine)
• selective serotonin reuptake inhibitors (SSRIs; e.g., citalopram, fluoxetine, paroxetine, sertraline)
• solifenacin
• thalidomide
• thiazide diuretics (water pills; e.g., hydrochlorothiazide, indapamide, metolazone)
• tiotropium
• tizanidine
• tolcapone
• tolterodine
• tramadol
• trazodone
• tricyclic antidepressants (e.g., amitriptyline, doxepin, imipramine, nortriptyline)
• triptan medications (e.g., eletriptan, frovatriptan, rizatriptan, sumatriptan)
• tryptophan
• umeclidinium
• vemurafenib
• verapamil
• zolpidem
• zopiclone
If you are taking any of these medications, speak with your doctor or pharmacist. Depending on your specific circumstances, your doctor may want you to:
• stop taking one of the medications,
• change one of the medications to another,
• change how you are taking one or both of the medications, or
• leave everything as is.
An interaction between two medications does not always mean that you must stop taking one of them. Speak to your doctor about how any drug interactions are being managed or should be managed.
Medications other than those listed above may interact with this medication. Tell your doctor or prescriber about all prescription, over-the-counter (non-prescription), and herbal medications you are taking. Also tell them about any supplements you take. Since caffeine, alcohol, the nicotine from cigarettes, or street drugs can affect the action of many medications, you should let your prescriber know if you use them.





