Gastroparesis Life Expectancy

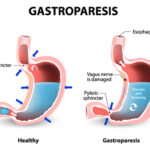
Gastroparesis is a medical condition that affects the normal movement and emptying of the stomach. The term “gastroparesis” comes from the Greek words “gastro” (stomach) and “paresis” (partial paralysis), indicating the partial paralysis of the stomach muscles.
This condition occurs when the muscles in the stomach wall become impaired or weakened, leading to delayed or incomplete digestion and emptying of food from the stomach into the small intestine. As individuals and their loved ones grapple with the impact of gastroparesis on daily life, questions about life expectancy and long-term outcomes often arise.
While gastroparesis itself does not directly affect life expectancy, its impact on overall health and well-being can be significant. In this article, we explore the factors that influence the quality of life for those living with gastroparesis and strategies to manage the condition effectively.
How common is gastroparesis?
Gastroparesis is considered a relatively rare condition, but its exact prevalence can be challenging to determine accurately. The reported prevalence varies depending on the population studied, the diagnostic criteria used, and the region or country surveyed. Additionally, some cases of gastroparesis may go undiagnosed or be misdiagnosed, further complicating the estimation of its true prevalence.
In the United States, gastroparesis is believed to affect around 0.2% to 2% of the population. However, this number might be underestimated since milder cases or cases with atypical symptoms may not be diagnosed. It is more commonly diagnosed in women than in men and tends to occur more frequently in older individuals.
The condition is often associated with underlying health conditions, most notably diabetes. In individuals with diabetes, the prevalence of gastroparesis is higher, with estimates ranging from 5% to 12%. Diabetes-related gastroparesis is termed diabetic gastroparesis and is a result of nerve damage (neuropathy) caused by high blood sugar levels over time.
While gastroparesis may be considered rare compared to other gastrointestinal conditions, its impact on affected individuals can be significant, leading to chronic symptoms and potential complications related to malnutrition and poor blood sugar control in diabetics. Early diagnosis and appropriate management are crucial for improving the quality of life for those living with gastroparesis.
Causes
Gastroparesis can be caused by various underlying factors, making it a complex and multifaceted condition. Some of the primary causes of gastroparesis include:
1. Diabetes: Diabetes mellitus, especially type 1 and type 2 diabetes, is one of the most common causes of gastroparesis. High blood sugar levels over time can damage the vagus nerve, which controls the movement of food through the digestive tract. This nerve damage can lead to impaired stomach motility and delayed gastric emptying.
2. Neurological Disorders: Gastroparesis can be a complication of certain neurological conditions, such as Parkinson’s disease, multiple sclerosis, and stroke. These conditions can affect the nerves that regulate stomach muscle contractions, leading to slowed gastric emptying.
3. Autoimmune Conditions: Autoimmune diseases, such as systemic lupus erythematosus or scleroderma, can lead to gastroparesis. In autoimmune disorders, the body’s immune system mistakenly attacks its own tissues, including the nerves and muscles in the stomach wall, disrupting the normal functioning of the digestive system.
4. Certain Medications: Some medications, particularly those that affect the central nervous system, can cause gastroparesis as a side effect. Opioid pain medications, certain antidepressants, and calcium channel blockers used to treat high blood pressure are examples of drugs that may contribute to delayed gastric emptying.
5. Post-Surgical Gastroparesis: In some cases, gastroparesis can develop after abdominal surgery, especially surgeries involving the stomach or vagus nerve. Surgical trauma can disrupt normal nerve signals and muscular functions, leading to delayed stomach emptying.
6. Viral Infections: Certain viral infections, such as herpes simplex virus, cytomegalovirus, and Epstein-Barr virus, have been associated with the development of gastroparesis. These infections may cause inflammation and damage to the nerves in the gastrointestinal tract.
7. Idiopathic Gastroparesis: When the exact cause of gastroparesis cannot be identified, it is termed idiopathic gastroparesis. This diagnosis is usually made after other potential causes have been ruled out through comprehensive medical evaluations.
What are the symptoms of gastroparesis?
Gastroparesis can cause a variety of symptoms, which can vary in severity and may come and go over time. Common symptoms of gastroparesis include:
1. Nausea: Persistent or chronic nausea is one of the hallmark symptoms of gastroparesis. The feeling of queasiness may be more pronounced after eating, and it can be distressing for individuals with the condition.
2. Vomiting: Gastroparesis can lead to frequent vomiting, which may occur shortly after eating or even several hours later. The vomit may contain undigested food.
3. Feeling Full Quickly: Patients with gastroparesis often experience early satiety, meaning they feel full very quickly after starting a meal, even after eating only a small amount of food.
4. Bloating: The delayed stomach emptying in gastroparesis can result in excessive gas and bloating in the abdomen, leading to discomfort and distension.
5. Abdominal Pain: Some individuals with gastroparesis may experience mild to moderate abdominal pain or discomfort. This pain may be intermittent or persistent.
6. Heartburn or Acid Reflux: Gastroparesis can contribute to gastroesophageal reflux disease (GERD) or worsen existing acid reflux symptoms due to the prolonged presence of stomach contents in the upper digestive tract.
7. Unintended Weight Loss: Due to reduced appetite and difficulty in consuming adequate amounts of food, gastroparesis can lead to unintended weight loss in some individuals.
8. Erratic Blood Sugar Levels: Gastroparesis can disrupt the normal digestion and absorption of nutrients, including carbohydrates. This can lead to unpredictable changes in blood sugar levels, especially in individuals with diabetes.
9. Malnutrition and Nutritional Deficiencies: Over time, gastroparesis can cause malnutrition and deficiencies in essential vitamins and minerals due to inadequate nutrient absorption.
10. Fluctuations in Blood Glucose Levels: For individuals with diabetes, gastroparesis can result in unpredictable fluctuations in blood glucose levels, making diabetes management more challenging.
It is essential to consult a healthcare professional if you experience persistent or recurrent symptoms of gastroparesis. Early diagnosis and proper management can help alleviate symptoms and prevent potential complications associated with the condition.
Treatment
The treatment of gastroparesis aims to alleviate symptoms, improve stomach motility, and enhance overall quality of life. The approach to treatment may vary depending on the severity of symptoms, underlying causes, and individual health status. Lifestyle modifications often form the foundation of treatment. Patients are advised to consume smaller, more frequent meals that are low in fat and fiber to ease digestion. Chewing food thoroughly and eating slowly can also aid in digestion. Avoiding large meals and refraining from lying down immediately after eating are recommended to prevent symptoms like nausea and reflux.
In addition to dietary changes, medications can be prescribed to promote gastric emptying and manage symptoms. Prokinetic agents, such as metoclopramide and domperidone, are commonly used to stimulate stomach contractions and speed up the passage of food through the digestive tract. Antiemetic medications may be given to control nausea and vomiting. In some cases, pain medications or antidepressants may also be prescribed to manage pain and discomfort associated with gastroparesis. For those with severe gastroparesis who are unable to tolerate oral nutrition, enteral nutrition through feeding tubes or parenteral nutrition (intravenous nutrition) may be considered to ensure adequate nutrient intake.
Life Expectancy and Underlying Causes
Gastroparesis itself is not a fatal condition, and individuals diagnosed with the disorder can have a normal life expectancy. However, the underlying causes of gastroparesis may have an impact on longevity. One of the most common underlying causes of gastroparesis is diabetes, particularly when poorly managed. High blood sugar levels over time can lead to nerve damage, including the vagus nerve, which controls stomach motility. Thus, individuals with diabetes and gastroparesis may face a higher risk of complications related to their diabetes, which could affect life expectancy if not well-managed.
Effect of Complications on Life Expectancy
While gastroparesis may not directly affect life expectancy, its potential complications can impact overall health. Delayed gastric emptying can lead to malnutrition and nutritional deficiencies due to reduced nutrient absorption. Prolonged exposure of stomach contents to stomach acid can also result in gastroesophageal reflux disease (GERD), which can damage the esophagus over time. Chronic vomiting and malnutrition may weaken the immune system, making individuals more susceptible to infections and other health issues.
In severe cases of gastroparesis, where nutritional intake is significantly impaired, individuals may require alternative methods of nutrition, such as feeding tubes or parenteral nutrition. Managing these complications effectively is essential for maintaining overall health and well-being, potentially influencing life expectancy in some cases.
Managing Gastroparesis and Improving Quality of Life
While there is no cure for gastroparesis, management strategies can help control symptoms, reduce complications, and improve the quality of life for individuals with the condition. Treatment options may include dietary modifications, such as consuming smaller, more frequent meals and avoiding foods that exacerbate symptoms. Medications can be prescribed to help stimulate stomach contractions and promote gastric emptying.
For those with diabetes-related gastroparesis, achieving and maintaining good blood sugar control is crucial. Working closely with healthcare providers, including gastroenterologists, dietitians, and diabetes specialists, is essential for developing personalized treatment plans tailored to the individual’s needs.
Conclusion
Gastroparesis, though not directly affecting life expectancy, can present significant challenges for those living with the condition. The underlying causes, such as diabetes, and potential complications, such as malnutrition, may have an impact on overall health and well-being. However, with proper management and lifestyle adjustments, individuals with gastroparesis can lead fulfilling lives and effectively manage symptoms to improve their quality of life. Seeking early diagnosis and appropriate treatment is vital to minimize complications and maintain optimal health for the long term. Support from healthcare professionals, family, and friends is essential for individuals navigating the complexities of living with gastroparesis.