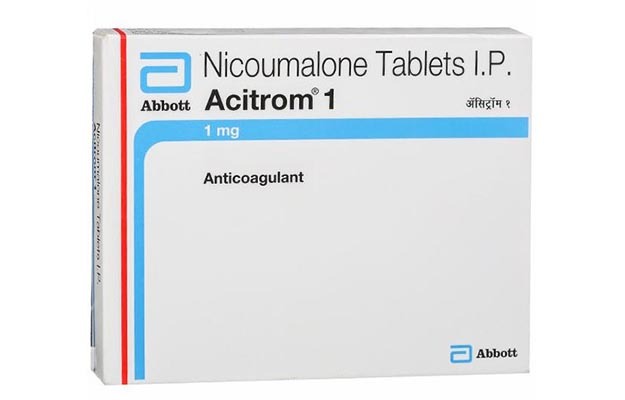
Acitorm: Composition, Uses, Dosage, Side Effects, Interactions
Acitorm is a brand of acenocoumarol (Nicoumalone) manufactured by Abbott. Acenocoumarol is a coumarin derivative used as an anticoagulant. Acitorm is used for the treatment and prevention of thromboembolic diseases. More specifically, it is indicated for the prevention of cerebral embolism, deep vein thrombosis, pulmonary embolism, thromboembolism in infarction, and transient ischemic attacks. It is used for the treatment of deep vein thrombosis and myocardial infarction. Acitorm is available in 0.5mg, 1mg, 2mg 3mg and 4mg. Generic brands of acenocoumarol are also available.
How Acitorm works
Acitorm (Acenocoumarol) works by inhibiting the reduction of vitamin K by vitamin K reductase which reduces the risk of blood clots forming inside the blood vessels. Blood clots normally only form to stop bleeding that has occurred as a result of injury to the tissues. The clotting process is complicated and begins when blood cells called platelets clump together at the site of damage and produce chemicals that activate clotting factors in the blood. Clotting factors are proteins that are produced by the liver. Vitamin K is essential for their production. The activated clotting factors cause a protein called fibrinogen to be converted into another called fibrin. Fibrin binds the platelets together, forming a blood clot. This is the body’s natural way of repairing itself.
Sometimes, however, a blood clot can form abnormally within the blood vessels. This is known as a thrombus and can be dangerous because the clot may detach and travel in the bloodstream, where it becomes known as an embolus. The clot may eventually get lodged in a blood vessel, thereby blocking the blood supply to a vital organ such as the heart, brain, or lungs. This is known as thromboembolism.
Some people have an increased tendency for blood clots to form within the blood vessels. This is usually due to a disturbance in the blood flow within the blood vessels. For example, fatty deposits on the walls of the blood vessels (atherosclerosis) can disrupt the blood flow, giving a tendency for platelets to clump together and start off the clotting process. Slow blood flow in the leg and pelvic veins can also result in clots forming (deep vein thrombosis). These clots can break off and travel to the lungs (pulmonary embolism). A type of fast irregular heartbeat called atrial fibrillation can also disrupt blood flow and may lead to blood clots forming in the heart. Heart valve disease can have the same effect, particularly if artificial heart valves have been fitted. Clots in the heart can detach and travel to the brain, causing a stroke. Acitorm is used to reduce the risk of blood clots forming inside the blood vessels in conditions such as these.
How to use Acitorm
• Take the Acitrom tablet as directed by your doctor.
• Swallow it as a whole with a glass of water, do not cut, break or chew the medicine.
• tablets are usually taken once a day. Take your dose at the same time each day.
• The dose that your doctor prescribes will vary from person to person and may vary from day to day. It depends on the condition being treated and your blood clotting time (INR or prothrombin time). You will need to have regular blood tests to check this and your doctor will adjust your dose based on the results. It is important to follow the instructions given by your doctor regarding how many tablets to take each day.
• The tablets can be taken either with or without food. They should be swallowed whole with a drink of water.
• If you forget to take a dose at your usual time take it as soon as you remember unless it is nearly time for your next dose. In this case, leave out the missed dose and take your next dose as usual when it is due. Do not take a double dose to make up for a missed dose.
• Keep taking this medicine every day as directed until your doctor tells you to stop.
What are the side effects of Acitorm?
- Bleeding and bruising.
- Increased time taken to stop bleeding.
- Decreased appetite.
- Nausea and vomiting.
- Hair loss (alopecia).
- Hypersensitivity reactions such as skin rashes or fever.
- Inflammation of blood vessels (vasculitis).
What other drugs could interact with Acitorm?
Acitorm can interact with any of the following drugs:
• alcohol
• allopurinol
• anticancer medications (e.g., carboplatin, cyclophosphamide, fluorouracil)
• azathioprine
• “azole” antifungals (e.g., fluconazole, ketoconazole, miconazole)
• barbiturates (e.g., primidone, phenobarbital)
• birth control pills
• carbamazepine
• cephalosporins (e.g., cefazolin, cefoperazone, cefotetan, cefoxitin)
• chloral hydrate
• chloramphenicol
• cholestyramine
• cimetidine
• clarithromycin
• clofibrate
• corticosteroids (e.g. prednisone, dexamethasone)
• danazol
• delavirdine
• dextran
• diazoxide
• diuretics (e.g. hydrochlorothiazide)
• erythromycin
• ethacrynic acid
• fenofibrate
• fluoxymesterone
• flutamide
• gemfibrozil
• glucagon
• griseofulvin
• halothane
• heparin and low-molecular-weight heparins (e.g. enoxaparin, dalteparin)
• herbs that affect blood clotting (e.g., St. John’s wort, ginseng, ginkgo Biloba, coenzyme Q10)
• lidocaine
• long-term use of narcotic pain medications (e.g. codeine, oxycodone, morphine, hydromorphone)
• MAO inhibitors (e.g., phenelzine, tranylcypromine)
• meprobamate
• mercaptopurine
• metronidazole
• mexilitine
• miconazole
• nonsteroidal anti-inflammatory drugs (NSAIDs; e.g., diclofenac, ibuprofen, naproxen, celecoxib, mefenamic acid)
• pentoxifylline
• phenylbutazone
• phenytoin
• potassium iodide
• primaquine
• propafenone
• propoxyphene
• propylthiouracil
• quinidine
• quinine
• quinolone antibiotics (e.g., ciprofloxacin, norfloxacin, ofloxacin)
• rifabutin
• rifampin
• salicylates (e.g., aminosalicylic acid, sodium salicylate, acetylsalicylic acid [ASA], methyl salicylate)
• selective serotonin reuptake inhibitors (SSRIs; e.g., duloxetine, fluoxetine, fluvoxamine, paroxetine, sertraline, citalopram)
• “statins” (e.g., fluvastatin, lovastatin, simvastatin)
• streptokinase
• sulfinpyrazone
• sulfonamides (e.g., sulfamethoxazole)
• sulfonylureas (e.g., glyburide, chlorpropamide, tolbutamide)
• tamoxifen
• tetracyclines (e.g., doxycycline, minocycline, tetracycline)
• thiabendazole
• thyroid hormones (e.g., levothyroxine, liothyronine, thyroid)
• ticlopidine
• tissue plasminogen activator (t-PA)
• urokinase
• vitamin E
• vitamin K
• warfarin
• zafirkulast.