Off-Label Drug Use: Meaning, Benefits, Risk, Regulation (50 Examples)

What does it mean when a drug is off-label?
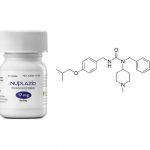
Off-label drug use is the use of medications for an indication or in an unapproved age group, dosage, or route of administration that has not been approved by the U.S. Food and Drug Administration (FDA). Both prescription drugs and over-the-counter drugs (OTCs) can be used in off-label ways, although most studies of off-label use focus on prescription drugs.
Off-label drug use is very common and generally legal unless it violates ethical guidelines or safety regulations. Off-label drug use can be motivated by several factors. First, a medication may not have been studied and approved for a specific population (eg, pediatric, geriatric, or pregnant patients). Second, a life-threatening or terminal medical condition may motivate a healthcare professional to give any treatment that is logical and available, whether approved by the FDA or not.
Third, if one medication from a class of drugs has FDA approval, physicians commonly use other medications in the same class without specific FDA approval for that use for the same indication. In addition, if the pathologic or physiologic features of 2 conditions are similar, a physician may use a medication approved for 1 of these conditions for both (eg, diabetes and metabolic syndrome; psychiatric diseases such as anxiety and posttraumatic stress disorder).
What is the difference between off-label and unlicensed?
Yes, unlicensed or unapproved drug use refers to the use of a medication that is legally approved or licensed in other countries, but not the US or UK. Most medications that fall under this category have to be imported because it is not available. Most times, these medicines are used for treating rare illnesses. The manufacturer may have decided that it was too expensive to carry out the clinical trials or it would be difficult to find enough patients for the clinical trials needed to secure approval or license.
What are the benefits of off-label drug use?
A drug is granted a license for use after a thorough assessment of risks and benefits based on high-quality scientific proof of its efficacy and safety. Off-label prescribing makes clinical sense only in exceptional circumstances. If reasonable evidence suggests that the benefit of off-label use will outweigh the risks, that declining to treat the condition poses even greater dangers than the off-label prescription does, and that there is no adequate alternative therapy, then off-label prescribing can benefit patients.
Prescribing off-label drugs gives medical practitioners more treatment options if one medication doesn’t work for you. It’s especially useful for rare conditions that have limited treatment options. For example, Off-label drug use makes it possible for chemotherapy approved to treat one type of cancer, to be used by healthcare providers to treat a different type of cancer.
How do I know that an “off-label” or unlicensed medicine is safe and will work?
Unlicensed and “off-label” medicines are only prescribed after careful consideration of other options available. Your doctors will have read information from medical publications supporting its use and may have taken advice from other experts. An unlicensed or “off-label” medicine will only be used if it is the most appropriate medicine for you and your illness or condition.
How do I know whether a medicine is unlicensed or being used “off-label”?
Your doctor or pharmacist will tell you that the medicine is not licensed or is being used off-label. The leaflet or insert that comes with the medicine may not say anything about how you should use it or may say that the medicine is not suitable for being used in the way we are prescribing it. This does not mean that it cannot be used safely to treat your condition – it means that the drug company does not have a license for using it in this way and so is not allowed to recommend this use.
What are the risks of off-label prescriptions?
Prescriptions for off-label uses of FDA-approved drugs are made without the benefit of an FDA-reviewed analysis of safety and effectiveness data. Physicians may resort to such prescribing to take advantage of new ideas and treatment approaches when available information to support them is inadequate. However, despite the potential risks associated with off-label uses, efforts to prohibit such uses might hurt the public. Some off-label prescribing may result because manufacturers have chosen not to invest the resources needed to have FDA add indications to the drug’s approval and labeling. A worst-case scenario for the nation’s health would be the widespread acceptance of a drug for off-label use that sufficient research would have revealed to be ineffective, unsafe or both.
Aside from the drug’s direct harm, the time spent waiting to see whether it worked would have been a time not spent exploring other treatment options. Unchecked off-label prescribing may also threaten the FDA gold standard of drug approval. If clinicians had already accepted a new use into practice through off-label prescribing, a manufacturer may choose to not invest resources to go through clinical trials and the FDA process to win approval. Although manufacturers do share information on off-label uses, courts have sometimes found they had overstepped allowable bounds.
How is Off-label drug regulated in the United States?
In the United States, once a drug has been approved for sale for one purpose, physicians are free to prescribe it for any other purpose that in their professional judgment is both safe and effective, and is not limited to official, FDA-approved indications. Pharmaceutical companies are not allowed to promote a drug for any other purpose without formal FDA approval. Marketing information for the drug will list one or more indications, that is, illnesses or medical conditions for which the drug has been shown to be both safe and effective.
This off-label prescribing is most commonly done with older, generic medications that have found new uses but have not had the formal (and often costly) applications and studies required by the FDA to formally approve the drug for these new indications. However, there is often extensive medical literature to support off-label use.
A leading example of how regulatory agencies approach off-label use is provided by the FDA’s Center for Drug Evaluation and Research, which reviews a company’s New Drug Application (NDA) for clinical trial data to see if the results support the drug for a specific use or indication. If satisfied that the drug is safe and effective, the drug’s manufacturer and the FDA agree on a specific language describing dosage, route of administration, and other information to be included on the drug’s label. More detail is included in the drug’s package insert.
Off-Label Drug Use Examples
1. Using the antidepressant Zoloft (sertraline) to treat social anxiety disorder
2. Using the antipsychotic Risperdal (risperidone) to treat attention deficit hyperactivity disorder (ADHD)
3. Using the anti-seizure medication Topamax (topiramate) to treat migraines
4. Using the antihistamine Benadryl (diphenhydramine) to treat insomnia
5. Using the muscle relaxant Soma (carisoprodol) to treat anxiety
6. Using the blood pressure medication Clonidine to treat Tourette’s Syndrome
7. Using the antihistamine Claritin (loratadine) to treat eczema
8. Using the antidepressant Wellbutrin (bupropion) to aid in smoking cessation
9. Using the anti-anxiety medication Xanax (alprazolam) to treat irritable bowel syndrome (IBS)
10. Using the antihypertensive medication Propranolol to treat stage fright or public speaking anxiety
11. Using the antipsychotic Seroquel (quetiapine) to treat insomnia
12. Using the antihistamine hydroxyzine to treat anxiety
13. Using the antidepressant Trazodone to treat insomnia
14. Using the antipsychotic Abilify (aripiprazole) to augment antidepressant treatment
15. Using the antihistamine Allegra (fexofenadine) to treat urticaria (hives)
16. Using the antidepressant Cymbalta (duloxetine) to treat chronic pain
17. Using the anti-seizure medication Gabapentin to treat anxiety
18. Using the muscle relaxant Baclofen to treat alcohol addiction
19. Using the antipsychotic Zyprexa (olanzapine) to treat anorexia nervosa
20. Using the antidepressant Remeron (mirtazapine) to stimulate appetite and treat weight loss
21. Using the antipsychotic Geodon (ziprasidone) to treat anxiety
22. Using the anti-inflammatory medication Celebrex (celecoxib) to prevent colon cancer
23. Using the anti-epileptic medication Lamictal (lamotrigine) to treat bipolar disorder
24. Using the muscle relaxant Flexeril (cyclobenzaprine) to treat chronic fatigue syndrome
25. Using the antidepressant Prozac (fluoxetine) to treat premature ejaculation
26. Using the antipsychotic Clozaril (clozapine) to treat refractory depression
27. Using the antihypertensive medication Clonidine to treat opioid withdrawal
28. Using the antipsychotic Haldol (haloperidol) to treat nausea and vomiting
29. Using the anti-seizure medication Neurontin (gabapentin) to treat restless leg syndrome
30. Using the antidepressant Effexor (venlafaxine) to treat hot flashes
31. Using the anti-inflammatory medication Aspirin to prevent heart attack
32. Using the antihistamine Atarax (hydroxyzine) to treat pruritus (itching)
33. Using the muscle relaxant Valium (diazepam) to treat muscle spasms
34. Using the antipsychotic Thorazine (chlorpromazine) to treat intractable hiccups
35. Using the anti-seizure medication Depakote (divalproex) to treat borderline personality disorder
36. Using the antidepressant Anafranil (clomipramine) to treat obsessive-comp
37. Using the antipsychotic Risperdal (risperidone) to treat autism spectrum disorder
38. Using the anti-seizure medication Keppra (levetiracetam) to treat bipolar disorder
39. Using the muscle relaxant Zanaflex (tizanidine) to treat tension headaches
40. Using the antihistamine Zyrtec (cetirizine) to treat allergic conjunctivitis
41. Using the antidepressant Paxil (paroxetine) to treat post-traumatic stress disorder (PTSD)
42. Using the antipsychotic Invega (paliperidone) to treat mood disorders
43. Using the anti-inflammatory medication Prednisone to treat autoimmune diseases
44. Using the antihistamine Doxepin to treat chronic urticaria
45. Using the anti-epileptic medication Lyrica (pregabalin) to treat generalized anxiety disorder
46. Using the muscle relaxant Robaxin (methocarbamol) to treat musculoskeletal pain
47. Using the antipsychotic Latuda (lurasidone) to treat bipolar depression
48. Using the antihistamine Periactin (cyproheptadine) to stimulate appetite and treat weight loss
49. Using the antidepressant Zoloft (sertraline) to treat postpartum depression
50. Using the anti-seizure medication Trileptal (oxcarbazepine) to treat neuropathic pain.