Morphine Immediate Release Vs Extended Release

Morphine is a prescription medicine used to treat acute pain. Morphine may be used alone or with other medications. Morphine belongs to a class of drugs called Opioid Analgesics. Opioids decrease pain by working on the brain to increase pain tolerance.
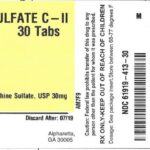
Morphine immediate release tablets relieves severe pain when less potent pain relievers are not effective. Morphine immediate release works quickly, it will usually relieve pain within about 30 minutes.
Sustained or extended-release pain relievers are only used when chronic pain control is necessary and should not be used to treat acute, or short-term pain. Your doctor may prescribe additional pain relievers that act more quickly for treatment of acute or “breakthrough” pain.
Dosage: Morphine Immediate Release Vs Extended Release
Morphine immediate-release tablets and capsules are used as ordered by your doctor. Read all information given to you. Follow all instructions closely. Take with or without food. Take with food if it causes an upset stomach.
Do not inject or snort this medicine (morphine immediate-release tablets and capsules). Doing any of these things can cause very bad side effects like trouble breathing and death from overdose.
Morphine also comes as a solution (liquid), an extended-release (long-acting) tablet, and as an extended-release (long-acting) capsule to take by mouth. The oral solution is usually taken every 4 hours as needed for pain. MS Contin brand and Arymo ER brand are extended-release tablets that are usually taken every 8 or every 12 hours. Morphabond brand extended-release tablets are usually taken every 12 hours. Kadian brand extended-release capsules are usually taken with or without food every 12 hours or every 24 hours. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand.
If you are taking morphine solution, use the dosing cup or syringe that comes with the medication to measure your dose. Be sure that you know how many milliliters of the liquid you should take. Ask your pharmacist if you have any question about how much medication you should take or how to use the dosing cup or syringe.
If you are taking Kadian brand extended-release capsules and you have a gastrostomy tube (surgically inserted feeding tube), ask your doctor or pharmacist how to administer the medication through your tube.
If you are unable to swallow the extended-release capsules (Kadian), you can carefully open a capsule, sprinkle all of the beads that it contains on a spoonful of cold or room temperature applesauce, and swallow the entire mixture immediately without chewing or crushing the beads. Then rinse your mouth with a little water and swallow the water to be sure that you have swallowed all the medication. Do not mix the beads into any other food. Do not save mixtures of medication and applesauce for later.
If you are taking the extended-release tablets (Arymo ER), swallow them one at a time with plenty of water. Swallow the extended-release tablets right after putting it in your mouth. Do not presoak, wet, or lick the extended-release tablets before you put them in your mouth.
Your doctor may start you on a low dose of morphine and gradually increase your dose until your pain is controlled. Your doctor may adjust your dose at any time during your treatment if your pain is not controlled. If you feel that your pain is not controlled, call your doctor. Do not change the dose of your medication without talking to your doctor.
Do not stop taking morphine without talking to your doctor. Your doctor may decrease your dose gradually. If you suddenly stop taking morphine, you may experience withdrawal symptoms such as restlessness; teary eyes; runny nose; yawning; irritability; anxiety; sweating; difficulty falling asleep or staying asleep; chills; back, muscle, or joint pain; nausea; vomiting; loss of appetite; diarrhea; stomach cramps; weakness; fast heartbeat; or fast breathing.
What are side effects of morphine immediate release and extended release?
The following side effects have been reported by at least 1% of people taking morphine immediate release and extended release. Many of these side effects can be managed, and some may go away on their own over time.
Contact your doctor if you experience these side effects and they are severe or bothersome. Your pharmacist may be able to advise you on managing side effects.
- changes in vision
- changes in sexual desire or activity
- confusion
- constipation
- decreased appetite
- difficult urination
- dizziness, lightheadedness, or feeling faint
- drowsiness
- dry mouth
- false sense of well-being
- headache
- itchiness
- loss of appetite
- irregular periods
- nausea
- nightmares or unusual dreams
- sweating
- trouble sleeping
- unusual tiredness or weakness
- vomiting
Although most of the side effects listed below don’t happen very often, they could lead to serious problems if you do not seek medical attention.
Check with your doctor as soon as possible if any of the following side effects occur:
- decreased coordination
- fast, slow, or pounding heartbeat
- hallucinations
- increased response to pain or burning sensations
- signs of blocked bowel (e.g., abdominal pain, severe constipation, nausea)
- skin rash
- withdrawal symptoms (e.g., nausea, vomiting, diarrhea, anxiety, shivering, cold and clammy skin, body aches, loss of appetite, sweating)
Stop taking this medication and seek medical attention immediately if any of the following occur:
- signs of overdose:
- cold, clammy skin
- confusion
- convulsions (seizures)
- dizziness (severe)
- drowsiness (severe)
- low blood pressure
- nervousness or restlessness (severe)
- pinpoint-sized pupils of eyes
- slow heartbeat
- slow or troubled breathing
- weakness (severe)
- signs of respiratory depression (e.g., slow, shallow, or weak breathing)
- signs of serious allergic reaction (e.g., abdominal cramps, difficulty breathing, nausea and vomiting, or swelling of the face and throat)
- symptoms of serotonin syndrome (e.g., confusion, fast heartbeat, hallucinations, restlessness, shaking, shivering, sudden jerking of muscles, sweating)
Some people may experience side effects other than those listed. Check with your doctor if you notice any symptom that worries you while you are taking this medication.
Are there any other precautions or warnings for this medication?
Before you begin using a medication, be sure to inform your doctor of any medical conditions or allergies you may have, any medications you are taking, whether you are pregnant or breast-feeding, and any other significant facts about your health. These factors may affect how you should use this medication:
Abdominal (stomach) conditions: Morphine and other narcotic medications may make the diagnosis of abdominal conditions more difficult or it may worsen these conditions. People who experience slower-than-normal passage of material through the digestive system may experience more side effects from morphine sustained release. If you have abdominal problems, discuss with your doctor how this medication may affect your medical condition, how your medical condition may affect the dosing and effectiveness of this medication, and whether any special monitoring is needed.
Accidental use: Accidental ingestion or use of as little as one dose of morphine by someone for whom it has not been prescribed can lead to a fatal overdose. Children are especially at risk. Keep this medication out of sight and reach of children.
Alcohol and other medications that cause drowsiness: Do not combine this medication with alcohol or other medications (e.g., antidepressants, sleeping pills, anxiety medications) that cause drowsiness since additional drowsiness or suppressed breathing can occur and be dangerous and possibly life-threatening.
Asthma and other respiratory conditions: Morphine may cause increased breathing difficulty for people having an acute asthma attack, or those with chronic obstructive pulmonary disease (chronic bronchitis, emphysema) or other conditions that affect breathing. If you have asthma or another breathing disorder, discuss with your doctor how this medication may affect your medical condition, how your medical condition may affect the dosing and effectiveness of this medication, and whether any special monitoring is needed.
Breathing: Morphine can suppress breathing, particularly if taken by someone who has not taken morphine before. This is a serious, potentially life-threatening condition. If you are at risk for breathing difficulties such as asthma, discuss with your doctor how this medication may affect your medical condition, how your medical condition may affect the dosing and effectiveness of this medication, and whether any special monitoring is needed. Keep this and all medications out of reach of children.
Dependence and withdrawal: Drug addiction is usually not a problem for people who require this medication for pain relief. Physical dependence (a need to take regular doses to prevent physical symptoms) has been associated with narcotic analgesics such as morphine. Withdrawal symptoms may be experienced if the dose is significantly reduced or suddenly discontinued. These symptoms include seizures, irritability, sleep problems, agitation, tremors, diarrhea, abdominal cramps, vomiting, headache, muscle cramps, extreme anxiety, tension, restlessness, sweating, and confusion. Reducing the dose gradually under medical supervision can help prevent or decrease these withdrawal symptoms when this medication is no longer required for pain control.
Dizziness: Morphine and other narcotics may cause dramatically reduced blood pressure, resulting in dizziness and unsteadiness. To reduce the possibility of severe dizziness, rise slowly when standing from a sitting or lying position.
Drowsiness/reduced alertness: Morphine may impair the mental or physical abilities needed for certain potentially hazardous activities such as driving a car or operating machinery. Avoid these activities until you know how this medication affects you.
Head injuries: Morphine can cause increased pressure inside the head. If you have an acute head injury or other conditions that increase your intracranial pressure (pressure inside the head), discuss with your doctor how this medication may affect your medical condition, how your medical condition may affect the dosing and effectiveness of this medication, and whether any special monitoring is needed.
Kidney function: Kidney disease or reduced kidney function may cause this medication to build up in the body, causing side effects. If you have reduced kidney function or kidney disease, discuss with your doctor how this medication may affect your medical condition, how your medical condition may affect the dosing and effectiveness of this medication, and whether any special monitoring is needed.
Low blood pressure: Morphine can cause low blood pressure or make low blood pressure worse. If you experience severe dizziness, especially when standing from a lying or sitting position, contact your doctor.
Liver function: If you have reduced liver function or liver disease, discuss with your doctor how this medication may affect your medical condition, how your medical condition may affect the dosing and effectiveness of this medication, and whether any special monitoring is needed.
Medical conditions: Morphine may cause increased symptoms or reduce the symptoms of worsening illness for people with Addison’s disease, reduced thyroid function, enlarged prostate, stricture of the urethra, reduced pituitary function, anemia, severe malnutrition, active ulcerative colitis, and hypothyroidism (low thyroid). If you have any of these conditions, discuss with your doctor how this medication may affect your medical condition, how your medical condition may affect the dosing and effectiveness of this medication, and whether any special monitoring is needed.
Seizures: Morphine may worsen preexisting seizure disorders. If tolerance to the medication develops and the dosage is increased substantially above recommended levels, seizures may occur in people without a history of seizure disorders. If you have a seizure disorder, discuss with your doctor how this medication may affect your medical condition, how your medical condition may affect the dosing and effectiveness of this medication, and whether any special monitoring is needed.
Serotonin syndrome: Severe reactions are possible when morphine is combined with other medications that act on serotonin, such as tricyclic antidepressants and serotonin reuptake inhibitors (medications used to treat depression). Symptoms of a reaction may include muscle rigidity and spasms, difficulty moving, or changes in mental state including delirium and agitation. Coma and death are possible.
If you are taking antidepressants, discuss with your doctor how this medication may affect your medical condition, how your medical condition may affect the dosing and effectiveness of this medication, and whether any special monitoring is needed.
Pregnancy: This medication should not be used during pregnancy unless the benefits outweigh the risks. If you become pregnant while taking this medication, contact your doctor immediately. Infants born to mothers who have been taking morphine for long periods of time or who are physically dependent on morphine will also be physically dependent on the medication and may experience breathing difficulties as well as withdrawal symptoms.
Breast-feeding: This medication passes into breast milk. If you are a breast-feeding mother and are taking morphine sustained release, it may affect your baby. Talk to your doctor about whether you should continue breast-feeding.
Children: Accidental ingestion of this medication by children may lead to severe and even fatal consequences. Keep this medication out of the reach of children.
Seniors: Seniors may be more sensitive to the effects of morphine and may require lower doses.
What other drugs could interact with this medication?
There may be an interaction between morphine and any of the following:
- aclidinium
- alcohol
- aldesleukin
- aliskiren
- alpha-agonists (e.g., clonidine, methyldopa)
- alpha-blockers (e.g., alfuzosin, doxazosin, tamsulosin)
- amiodarone
- amphetamines (e.g., dextroamphetamine, lisdexamfetamine)
- angiotensin converting enzyme inhibitors (ACEIs; captopril, enalapril, ramipril)
- angiotensin receptor blockers (ARBs; e.g., candesartan, irbesartan, losartan)
- antihistamines (e.g., cetirizine, doxylamine, diphenhydramine, hydroxyzine, loratadine)
- antipsychotics (e.g., chlorpromazine, clozapine, haloperidol, olanzapine, quetiapine, risperidone)
- atropine
- azelastine
- “azole” antifungals (e.g., itraconazole, ketoconazole, voriconazole)
- barbiturates (e.g., butalbital, pentobarbital, phenobarbital)
- belladonna
- benzodiazepines (e.g., alprazolam, diazepam, lorazepam)
- beta-blockers (e.g., atenolol, metoprolol, propranolol)
- benztropine
- bromocriptine
- buprenorphine
- buspirone
- butorphanol
- calcium channel blockers (e.g., amlodipine, diltiazem, nifedipine, verapamil)
- cannabis
- chloral hydrate
- clopidogrel
- cyclosporine (systemic)
- darifenacin
- desmopressin
- dexamethasone
- disopyramide
- diuretics (water pills; e.g., furosemide, hydrochlorothiazide, triamterene)
- domperidone
- dronedarone
- efavirenz
- elagolix
- eluxadoline
- entacapone
- flavoxate
- flibanserin
- general anesthetics (medications used to put people to sleep before surgery)
- glycopyrrolate
- ipratropium
- ketotifen
- lapatinib
- linezolid
- methylene blue
- metoclopramide
- mirtazapine
- monoamine oxidase inhibitors (MAOIs; e.g., moclobemide, phenelzine, rasagiline, selegiline, procarbazine, tranylcypromine) taken within the past 14 days
- muscle relaxants (e.g., baclofen, cyclobenzaprine, methocarbamol, orphenadrine)
- nabilone
- naltrexone
- nitrates (e.g., nitroglycerin, isosorbide dinitrate, isosorbide mononitrate)
- obinutuzumab
- octreotide
- other narcotic analgesics (e.g., codeine, fentanyl, meperidine, oxymorphone)
- oxybutynin
- pegvisomant
- phosphodiesterase 5 inhibitors (e.g., sildenafil, tadalafil, vardenafil)
- pramipexole
- prasugrel
- quinidine
- quinine
- reserpine
- rifabutin
- rifampin
- ropinirole
- rotigotine
- sacubitril
- St. John’s wort
- scopolamine
- seizure medications (e.g., carbamazepine, clobazam, levetiracetam, phenobarbital, phenytoin, primidone, topiramate, valproic acid, zonisamide)
- selective serotonin reuptake inhibitors (SSRIs; e.g., citalopram, fluoxetine, paroxetine, sertraline)
- serotonin/norepinephrine reuptake inhibitors (SNRIs; e.g., desvenlafaxine, duloxetine, venlafaxine)
- sodium oxybate
- solifenacin
- tapentadol
- tenofovir
- thalidomide
- ticagrelor
- ticlopidine
- tiotropium
- tolcapone
- tolterodine
- tramadol
- trazodone
- tricyclic antidepressants (e.g., amitriptyline, clomipramine, desipramine, trimipramine)
- umeclidinium
- zolpidem
- zopiclone
If you are taking any medications that have a sedating effect, speak with your doctor or pharmacist. Depending on your specific circumstances, your doctor may want you to:
- stop taking one of the medications,
- change one of the medications to another,
- change how you are taking one or both of the medications, or
- leave everything as is.
An interaction between two medications does not always mean that you must stop taking one of them. In many cases, interactions are intended or are managed by close monitoring. Speak to your doctor about how any drug interactions are being managed or should be managed.
Medications other than those listed above may interact with this medication. Tell your doctor or prescriber about all prescription, over-the-counter (non-prescription), and herbal medications that you are taking. Also tell them about any supplements you take. Since caffeine, alcohol, the nicotine from cigarettes, or street drugs can affect the action of many medications, you should let your prescriber know if you use them.