How Does Antibiotic Resistance Occur
What is antibiotic resistance?
Antibiotic resistance, also known as antimicrobial resistance (AMR), is a significant public health concern characterized by the ability of bacteria, viruses, parasites, and other microorganisms to evolve and adapt, making the drugs designed to kill or inhibit their growth less effective. In the case of bacteria, this means they can survive and continue to grow in the presence of antibiotics that were once effective in treating infections caused by them.
Antibiotic resistance is a complex and ongoing phenomenon that has developed over the course of several decades.
Historical Timelines
1. Pre-Antibiotic Era (Before 1928): Before the discovery of antibiotics, infectious diseases were a leading cause of death worldwide. Infections that we consider minor today, like strep throat or a simple cut, could be life-threatening.
2. 1928 – Discovery of Penicillin: Sir Alexander Fleming’s discovery of penicillin in 1928 marked the beginning of the antibiotic era. This revolutionary drug saved countless lives and was the first widely used antibiotic.
3. 1940s – Golden Age of Antibiotics: During and after World War II, many new antibiotics were discovered and developed, including streptomycin and tetracycline. These drugs were highly effective against a wide range of bacteria, and their use became widespread.
4. 1950s – Early Signs of Resistance: The first cases of antibiotic resistance were reported, mainly in hospitals. Bacteria were found to develop resistance to antibiotics, particularly in settings where antibiotics were used extensively.
5. 1960s – Overuse and Misuse: The overuse and misuse of antibiotics in medicine, agriculture, and veterinary practices became more widespread. This further accelerated the development of antibiotic resistance.
6. 1970s – Multidrug Resistance: Bacteria began to exhibit resistance to multiple antibiotics. The term “superbug” was coined to describe these strains of bacteria that were difficult to treat.
7. 1980s – The Antibiotic Pipeline Slows: Fewer new antibiotics were being discovered and developed, leading to a decline in the number of effective drugs available.
8. 1990s – Methicillin-Resistant Staphylococcus aureus (MRSA): MRSA emerged as a significant public health threat. This strain of Staphylococcus aureus was resistant to many commonly used antibiotics.
9. 2000s – Growing Concern: Antibiotic resistance became a major global health concern. Various international organizations and governments began to take action to address the issue.
10. 2010s – Antimicrobial Stewardship: Efforts to promote responsible antibiotic use, known as antimicrobial stewardship, gained prominence. There was an increased focus on preventing infections and reducing antibiotic overuse.
11. 2020s – The Ongoing Challenge: Antibiotic resistance remains a serious global health threat. New antibiotics are still being developed, but the pace is slow compared to the emergence of resistant bacteria. The COVID-19 pandemic also highlighted the importance of antibiotics in managing secondary bacterial infections.
What causes antibiotic resistance?
Antibiotic resistance is primarily caused by the overuse and misuse of antibiotics, which allows bacteria to adapt and develop resistance. Here are the key factors and mechanisms that contribute to antibiotic resistance:
1. Bacterial Mutations: Bacteria can naturally mutate over time. These mutations can lead to changes in their genetic makeup, including the genes responsible for antibiotic susceptibility. Some mutations may confer resistance to antibiotics, allowing the bacteria to survive and reproduce in the presence of the drug.
2. Selection Pressure: When antibiotics are used to treat infections, they create a selection pressure on bacteria. This means that only the bacteria with resistance mechanisms or mutations survive the antibiotic treatment, while susceptible bacteria are killed. This selective advantage for resistant bacteria is a driving force behind the development of resistance.
3. Overuse and Misuse of Antibiotics: Inappropriate use of antibiotics, such as taking them when they are not needed, not completing a full course of treatment, or using antibiotics for viral infections (which they don’t treat), contributes to the development of resistance. Overuse and misuse of antibiotics provide more opportunities for bacteria to develop and spread resistance.
4. Incomplete Treatment: Not completing the full prescribed course of antibiotics can leave surviving bacteria with a partial resistance, allowing them to adapt and develop stronger resistance in the future.
5. Widespread Use in Agriculture: Antibiotics are often used in agriculture to promote growth in livestock and prevent disease. This agricultural use can lead to the spread of antibiotic-resistant bacteria through food products and the environment.
6. Transmission of Resistant Bacteria: Resistant bacteria can be transmitted from person to person, either directly or indirectly through contact with contaminated surfaces or through the food chain. Hospitals, in particular, can be hotspots for the spread of resistant bacteria.
7. Inadequate Infection Control: Poor infection control practices in healthcare settings can lead to the transmission of resistant bacteria. This includes inadequate hand hygiene, improper disinfection of medical equipment, and crowded healthcare facilities.
8. Lack of Development of New Antibiotics: The antibiotic pipeline has slowed down in terms of the development of new antibiotics. This means that there are fewer treatment options available for infections caused by resistant bacteria.
9. Biofilm Formation: Some bacteria can form biofilms, which are protective structures that make them less susceptible to antibiotics. Biofilms can be found in various environments, including medical devices like catheters and prosthetic joints.
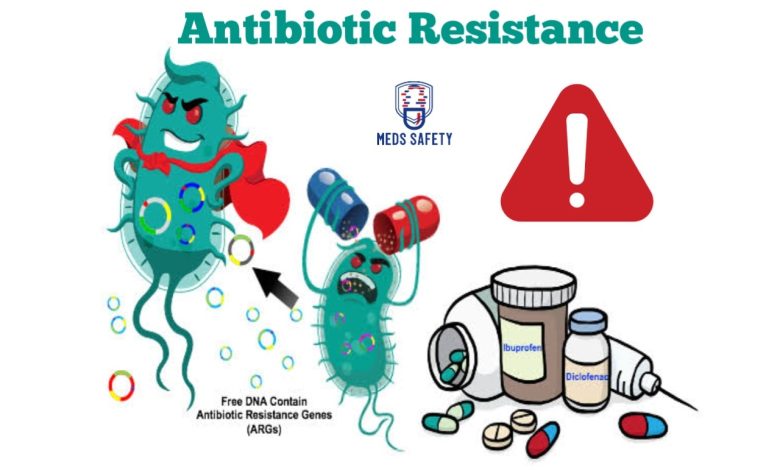
10. Horizontal Gene Transfer: Bacteria can share resistance genes with each other through mechanisms like plasmid transfer. This allows the rapid spread of resistance in bacterial populations.
What are the 5 mechanisms of antibiotic resistance?
Antibiotic resistance can occur through various mechanisms, and bacteria can develop resistance to antibiotics in several ways. Here are five key mechanisms of antibiotic resistance:
1. Enzymatic Degradation or Modification: Bacteria can produce enzymes that degrade or modify antibiotics. For example, beta-lactamase enzymes can break down beta-lactam antibiotics like penicillin. By modifying the antibiotic, the bacteria render it ineffective.
2. Altered Target Sites: Some bacteria can modify the target sites that antibiotics bind to. This alteration can prevent the antibiotic from binding to its intended target, making it ineffective. For instance, methicillin-resistant Staphylococcus aureus (MRSA) has modified penicillin-binding proteins, making it resistant to beta-lactam antibiotics.
3. Efflux Pumps: Bacteria can have efflux pumps that actively pump antibiotics out of the bacterial cell. This reduces the concentration of the antibiotic within the cell, preventing it from reaching a level that can effectively inhibit bacterial growth. Efflux pumps are particularly common in Gram-negative bacteria like Escherichia coli.
4. Reduced Permeability: Some bacteria can reduce their outer membrane permeability to limit the entry of antibiotics into the cell. This is often seen in Gram-negative bacteria, which have an outer membrane that acts as a barrier. By restricting the antibiotic’s entry, the bacteria make it less effective.
5. Target Mimicry: Bacteria can develop proteins that mimic the target sites of antibiotics, diverting the drugs away from their intended targets. This mechanism, known as target mimicry, can render antibiotics ineffective by preventing them from acting on their intended target.
These are just a few of the mechanisms bacteria can use to develop resistance to antibiotics. Importantly, bacteria can often employ multiple mechanisms simultaneously, making them highly adaptable and capable of resisting multiple classes of antibiotics. This underscores the need for responsible antibiotic use and the development of new antibiotics to combat these mechanisms of resistance.
Examples of antibiotic resistance
Antibiotic resistance can be observed in various bacterial strains and across a wide range of antibiotics. Here are some examples of antibiotic-resistant bacteria and the antibiotics to which they have developed resistance:
1. Methicillin-Resistant Staphylococcus aureus (MRSA): MRSA is a well-known example of antibiotic resistance. It is resistant to beta-lactam antibiotics, such as methicillin, penicillin, and cephalosporins. MRSA infections can be challenging to treat and are a significant concern in healthcare settings.
2. Extended-Spectrum Beta-Lactamase (ESBL)-Producing Enterobacteriaceae: These bacteria, including strains of Escherichia coli and Klebsiella pneumoniae, produce enzymes called ESBLs that confer resistance to a broad range of beta-lactam antibiotics, including penicillins and cephalosporins.
3. Vancomycin-Resistant Enterococci (VRE): Enterococci are bacteria that have become resistant to vancomycin, a powerful antibiotic often used as a last resort for treating serious infections. VRE can cause difficult-to-treat healthcare-associated infections.
4. Carbapenem-Resistant Enterobacteriaceae (CRE): CRE includes bacteria like Klebsiella pneumoniae and Escherichia coli that have developed resistance to carbapenem antibiotics, which are some of the most potent antibiotics available for treating serious bacterial infections.
5. Fluoroquinolone-Resistant Gonorrhea: Some strains of Neisseria gonorrhoeae, the bacterium responsible for gonorrhea, have developed resistance to fluoroquinolone antibiotics. This complicates the treatment of this sexually transmitted infection.
6. Tuberculosis (TB) with Multidrug Resistance (MDR-TB): Mycobacterium tuberculosis, the bacterium that causes TB, can develop resistance to multiple antibiotics, leading to MDR-TB. Treatment of MDR-TB is more complex and requires a longer course of antibiotics.
7. Clostridium difficile (C. difficile) with Resistance to Multiple Antibiotics: C. difficile is a bacterium that can cause severe gastrointestinal infections. Some strains have developed resistance to multiple antibiotics, making the treatment of C. difficile infections more challenging.
8. Acinetobacter baumannii with Resistance to Multiple Antibiotics: Acinetobacter baumannii is an opportunistic pathogen that has developed resistance to various antibiotics, including carbapenems and aminoglycosides. It is often associated with healthcare-associated infections.
These examples highlight the diversity of antibiotic resistance in different bacterial species and the impact it can have on healthcare and public health. They underscore the need for responsible antibiotic use, infection control measures, and the development of new antibiotics to address the growing challenge of antibiotic resistance.
How long does antibiotic resistance last?
Antibiotic resistance is a complex and ongoing process, and it doesn’t have a fixed duration. Instead, it can persist for a variable amount of time and may even be considered permanent in certain cases. The duration and persistence of antibiotic resistance depend on several factors:
1. Genetic Mutations: Antibiotic resistance often arises from genetic mutations in the bacteria. Once these mutations occur, they are typically passed on to subsequent generations of bacteria. This can make resistance a long-lasting trait within a bacterial population.
2. Selective Pressure: The presence of antibiotics creates selective pressure. Bacteria with resistance mechanisms have a survival advantage in the presence of antibiotics because they can survive and reproduce, while susceptible bacteria are killed. As long as antibiotics are used, this selective pressure can maintain and even reinforce resistance.
3. Transfer of Resistance: In some cases, bacteria can transfer genetic material, including antibiotic resistance genes, to other bacteria through mechanisms like horizontal gene transfer. This means that resistance genes can spread to different bacterial species, potentially perpetuating resistance over time.
4. Antibiotic Use and Misuse: The frequency and patterns of antibiotic use significantly impact the duration of antibiotic resistance. Overuse and misuse of antibiotics can accelerate the development and persistence of resistance. Reducing or altering antibiotic use can slow down the spread of resistance.
5. Microbial Ecology: The duration of antibiotic resistance can vary depending on the ecological context. Bacteria exist in complex communities, and factors such as competition, interactions with other microorganisms, and environmental conditions can influence the persistence of resistance.
Antibiotic resistance can persist and evolve as long as the conditions that drive its development and maintenance are present. These conditions include the use of antibiotics, the presence of selective pressures, and the genetic mechanisms that confer resistance. To mitigate antibiotic resistance, responsible antibiotic use, infection prevention measures, and the development of new antibiotics are crucial in managing and reducing its impact.
How to prevent antibiotic resistance
Preventing antibiotic resistance is a critical global health goal, and it requires coordinated efforts from healthcare providers, policymakers, and the public. Here are several strategies to help prevent antibiotic resistance:
1. Use Antibiotics Responsibly:
• Take antibiotics only when prescribed by a healthcare professional.
• Follow the prescribed dosage and complete the entire course, even if you start feeling better.
• Never share antibiotics with others or use leftover antibiotics from previous treatments.
2. Practice Good Infection Control:
• Practice good hygiene, including regular handwashing with soap and water.
• Follow proper food safety measures to prevent foodborne illnesses.
• Get vaccinated to prevent vaccine-preventable diseases.
• Stay home when you’re sick to avoid spreading infections to others.
3. Prevent Infections:
• Use preventive measures like condoms to reduce the risk of sexually transmitted infections.
• Maintain good oral hygiene to prevent dental infections.
• Avoid close contact with people who have contagious infections.
4. Promote Vaccination:
• Vaccines can prevent many bacterial and viral infections, reducing the need for antibiotics. Stay up-to-date on recommended vaccines.
5. Reduce Antibiotic Use in Agriculture:
• Support policies and practices that limit the use of antibiotics in livestock for growth promotion and disease prevention. This can reduce the emergence of antibiotic-resistant bacteria in food sources.
6. Support Research and Development:
• Invest in the development of new antibiotics to replace older, less effective ones. The antibiotic pipeline is running dry, and new drugs are needed to combat resistance.
7. Implement Infection Control Measures in Healthcare Settings:
• Hospitals and healthcare facilities should have robust infection control protocols to prevent the spread of drug-resistant bacteria.
• Isolate patients with drug-resistant infections to prevent transmission.
8. Track and Monitor Resistance:
• Surveillance systems should monitor the prevalence of antibiotic-resistant infections and provide data to guide treatment decisions.
9. Educate Healthcare Professionals and the Public:
• Healthcare providers should be educated about responsible antibiotic prescribing.
• Public awareness campaigns can inform people about the risks of antibiotic resistance and the importance of using antibiotics appropriately.
10. Wash Your Hands:
• Regular and thorough handwashing with soap and water is one of the most effective ways to prevent the spread of infections.
Preventing antibiotic resistance is a complex, multifaceted effort that requires the collaboration of individuals, healthcare providers, governments, and researchers. By following these guidelines and promoting responsible antibiotic use, we can help slow down the development and spread of antibiotic-resistant bacteria, preserving the effectiveness of these life-saving drugs.





