Examples Of Nondihydropyridine Calcium Channel Blockers & Their Side Effects

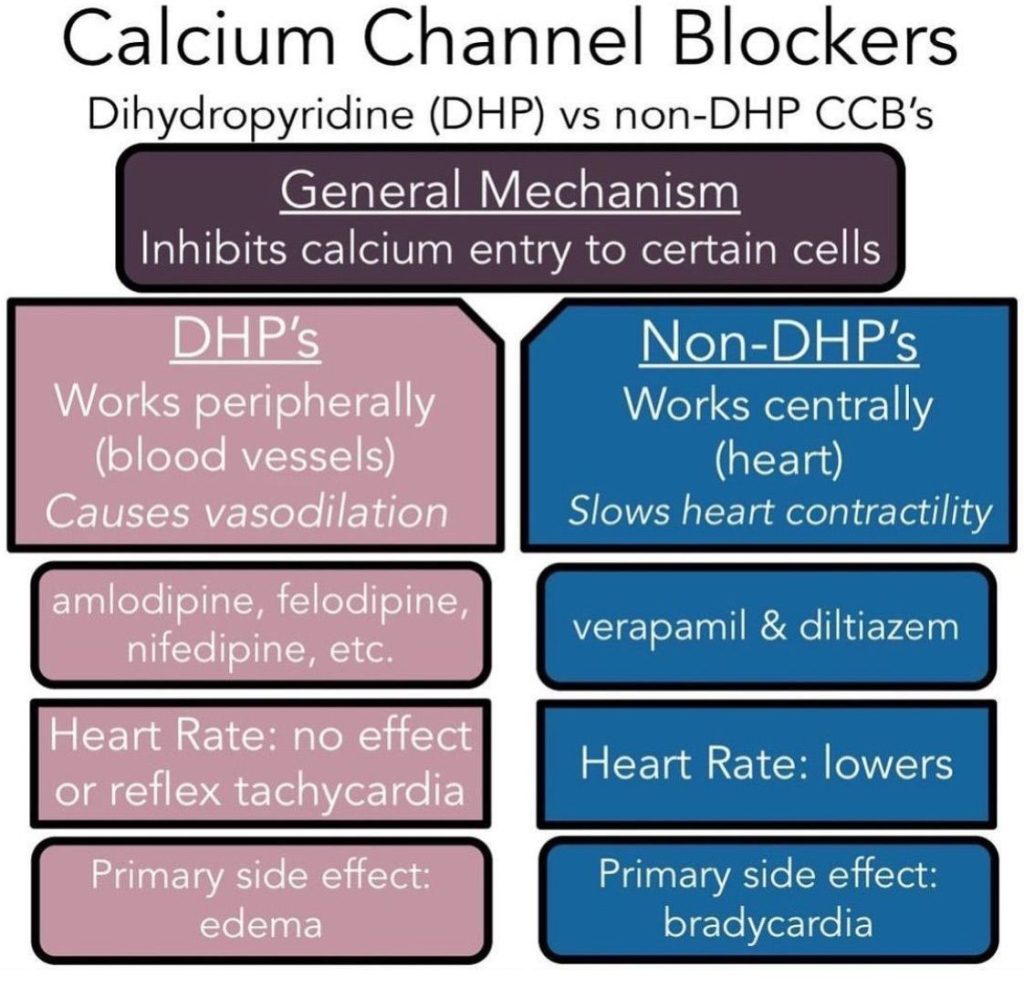
Nondihydropyridine calcium channel blockers (NDHP CCBs) constitute a critical class of pharmaceutical agents employed predominantly in the management of cardiovascular disorders. Their primary mechanism of action involves the inhibition of calcium ion influx into cardiac and smooth muscle cells, exerting diverse effects on the cardiovascular system. By targeting L-type calcium channels, NDHP CCBs modulate cellular calcium concentrations, resulting in alterations to muscle contractility. This nuanced impact extends to the heart’s conduction system, particularly affecting the sinoatrial (SA) and atrioventricular (AV) nodes. This characteristic distinguishes NDHP CCBs from their dihydropyridine counterparts, underscoring the importance of understanding the chemical variances and functional disparities within the calcium channel blocker class.
Within the broader category of calcium channel blockers, dihydropyridines and nondihydropyridines represent distinct subgroups. While both share the commonality of inhibiting calcium influx, the specific effects and applications differ. Dihydropyridines primarily influence peripheral vascular resistance, offering potent vasodilation, whereas nondihydropyridines, exert more pronounced effects on cardiac tissue. This divergence in pharmacological action makes NDHP CCBs particularly valuable in the treatment of conditions requiring modulation of heart rate and rhythm.
This article will delve into examples of NDHP CCBs, exploring their mechanisms of action, therapeutic uses, and potential side effects. Understanding these medications is crucial for both healthcare professionals and patients as they play a pivotal role in treating various cardiovascular disorders.
Nondihydropyridine Calcium Channel Blockers Vs Dihydropyridine
Dihydropyridine calcium channel blockers primarily exert vasodilatory effects in the peripheral regions, while nondihydropyridine calcium channel blockers distinctly influence the sinoatrial (SA) and atrioventricular (AV) nodes, potentially causing myocardial depression alongside limited peripheral vasodilation.
Examples Of Nondihydropyridine Calcium Channel Blockers
Here are some examples of nondihydropyridine calcium channel blockers:
1. Verapamil: Verapamil is a nondihydropyridine calcium channel blocker prescribed for a range of cardiovascular conditions, including angina, hypertension, and certain arrhythmias. Its mechanism of action centers on inhibiting calcium influx into cardiac and smooth muscle cells. By doing so, verapamil exerts a direct influence on contractility and conduction within the heart. This dual effect makes it a valuable medication for conditions where controlling both blood pressure and heart rhythm is essential.
2. Diltiazem: Diltiazem is another notable nondihydropyridine calcium channel blocker utilized in the treatment of angina, high blood pressure, and specific heart rhythm disorders. Its mechanism of action involves the blockade of calcium channels in both the heart and blood vessels. This action leads to a reduction in contractility, easing the workload on the heart, and induces vasodilation, thereby contributing to its antihypertensive effects. Diltiazem’s versatility in addressing various cardiovascular issues underscores its significance in clinical practice.
3. Bepridil: Bepridil, though less commonly prescribed, plays a crucial role in managing angina and certain arrhythmias. Its mechanism of action sets it apart by exhibiting antianginal and antiarrhythmic properties through its impact on calcium channels. Despite its less frequent use, bepridil’s unique combination of therapeutic effects makes it a valuable option in specific cases where its distinct actions are advantageous.
4. Gallopamil: Gallopamil is employed in certain countries for treating angina and specific heart rhythm disturbances. Its therapeutic effects are attributed to its action on calcium channels. By modulating calcium entry, gallopamil contributes to the medication’s effectiveness in addressing cardiovascular issues. While not as widely recognized as some other NDCCBs, its inclusion in the pharmacological toolkit speaks to its utility in managing particular cardiac conditions.
5. Fendiline: Fendiline, though not as commonly prescribed, possesses noteworthy antianginal and antiarrhythmic properties. Its mechanism of action involves the modulation of calcium channels, impacting both cardiac function and rhythm. Despite its relative underuse, fendiline’s unique attributes make it a consideration in cases where its specific actions align with the therapeutic goals for individual patients.
6. Lercanidipine: Primarily classified as a dihydropyridine, lercanidipine exhibits some nondihydropyridine characteristics and is utilized primarily for hypertension. Its mechanism of action involves influencing calcium entry into cells, contributing to its antihypertensive effects. While not a classic NDCCB, lercanidipine’s inclusion here underscores the diversity within the calcium channel blocker class and highlights its role in managing hypertension, showcasing the nuanced approach required in cardiovascular pharmacotherapy.
Side Effects of Nondihydropyridine Calcium Channel Blockers
While NDHP CCBs are generally well-tolerated, they can cause side effects that vary in severity. It’s crucial for healthcare providers and patients to be aware of potential adverse reactions.
• Hypotension: One common side effect is low blood pressure, which may lead to dizziness or fainting. Patients should be advised to stand up slowly from a sitting or lying position to minimize the risk of orthostatic hypotension.
• Bradycardia: Due to their impact on the heart’s conduction system, NDHP CCBs can cause bradycardia (slow heart rate). This effect may be more pronounced in individuals with pre-existing heart conditions.
• Constipation: Verapamil, in particular, is known to cause constipation. Patients should maintain adequate hydration and consider dietary adjustments to alleviate this side effect.
• Edema: Peripheral edema (swelling of the extremities) can occur with the use of NDHP CCBs. This is thought to be related to their vasodilatory effects and increased capillary permeability.
• Gastrointestinal Effects: Nausea, vomiting, and abdominal discomfort are reported in some individuals. These symptoms are usually mild but may warrant a change in medication or dose adjustment.
• Conduction Abnormalities: NDHP CCBs, especially verapamil, may cause conduction abnormalities, including heart block. Close monitoring of cardiac function is essential, especially in patients with pre-existing conduction disorders.
• Drug Interactions: NDHP CCBs can interact with other medications, leading to potentially serious consequences. For instance, concurrent use with beta-blockers may exacerbate bradycardia, and combining them with certain antiarrhythmic drugs may increase the risk of adverse effects.
• Hepatotoxicity: Rarely, NDHP CCBs have been associated with liver dysfunction. Patients should be monitored for signs of hepatic impairment, such as jaundice and elevated liver enzymes.
Monitoring and Precautions
• Regular monitoring of blood pressure and heart rate is essential during NDHP CCB therapy.
• Patients with pre-existing heart conditions, especially conduction abnormalities, may require closer supervision.
• Healthcare providers should be cautious when prescribing NDHP CCBs to patients with impaired liver function.
• Patient education is crucial, emphasizing the importance of adherence to prescribed medications, recognizing and reporting side effects, and understanding the significance of regular follow-up appointments.
Conclusion
Nondihydropyridine calcium channel blockers play a vital role in the management of various cardiovascular conditions, offering effective solutions for hypertension, angina, and certain arrhythmias.
While generally well-tolerated, healthcare providers and patients must be aware of potential side effects and take necessary precautions. Regular monitoring and open communication between patients and their healthcare teams are key to ensuring the safe and effective use of these medications in promoting cardiovascular health.





