Drug-induced Psychosis: List, Causes, Symptoms, Treatment

What is Drug-induced psychosis?
Drug-induced psychosis, commonly known as stimulant psychosis is defined as any psychotic episode which has been caused by abuse of stimulants, an adverse reaction to prescription drugs, or excessive use of alcohol which has directly triggered a psychotic reaction. These psychoses are categorized into three classifications of symptoms: positive, negative, and cognitive. The symptoms of Drug-induced psychosis are not different from the symptoms of schizophrenia and it is difficult to distinguish between them.
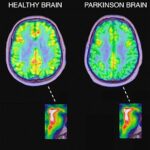
Due to this ambiguity of distinction between the Drug-induced psychosis and schizophrenia, the DIP animal model has been frequently used as the schizophrenia animal model. However, although the symptoms may be the same, its causes are clearly different in that Drug-induced psychosis is acquired and schizophrenia is heritable.
How does drug-induced psychosis happen?
Drug-induced psychosis can happen when you take too much of a certain drug, so that its level of toxicity provokes paranoia and a psychotic episode. It can also occur when you have an adverse reaction from mixing different substances, or withdrawing from a drug, prescribed or otherwise. You may already have underlying mental health conditions such as bipolar disorder or schizophrenia, where delusions and hallucinations are associated symptoms, with psychotic episodes resulting from substance use, indicating that you may be prone to psychosis.
If your psychosis has been triggered through drug use in order to cope with underlying mental illness, a diagnosis would need to determine whether symptoms would continue without the drug present, as this would not be drug-related psychosis. Drug-induced psychosis is more apparent when your symptoms wear off after you have stopped using the drug, while the initial symptoms such as social withdrawal and lack of motivation may gradually build to include delusions or hallucinations.
What are the drugs that can cause Psychosis?
Heavy, long-term use of many substances can result in psychotic symptoms. However, certain drugs are more likely to cause psychotic symptoms than others. These include:
Prescription meds (e.g., ketamine): Ketamine users typically exhibit a variety of symptoms that mimic psychosis including delusions, cognitive impairments, disordered thinking, and incoherent speech.
Cannabis: The use of cannabis has long been associated with psychotic symptoms. The first evidence came from the Swedish Conscripts Study of 45,570 military inductees who were followed-up for 15 years. The results showed that those who had used cannabis by the age of 17 were 2.4 times more likely to develop schizophrenia than non-users. The risk of schizophrenia rose to 6 times that of non-users for heavy cannabis users (more than 50 times at initial interview)
Cocaine: Up to 50% of cocaine users will show some symptoms of psychosis after use. The risk increases with needle or freebased use. Persecution delusions and tactile hallucinations are common. Psychotic symptoms can persist for days, months, and sometimes years after use has stopped.
Amphetamine: Amphetamine (Speed) can cause psychotic symptoms similar to methamphetamine and cocaine after repeated use.
Alcohol: Alcohol can cause delusions, mental confusion, disorganized speech, and disorientation. Typically, these symptoms subside upon sobriety. Alcohol is one of the most commonly abused substances among individuals with schizophrenia, although diagnosis usually precedes use.
Methamphetamine: The use of methamphetamine can lead to paranoia, persecution delusions, auditory and visual hallucinations. One common hallucination is the feeling of bugs crawling on one’s skin. These symptoms might subside after stopping use, but they can also persist for weeks or longer, and may increase one’s susceptibility for developing future psychosis. Even after long periods of abstinence, psychotic symptoms may return in periods of stress.
Psychedelic drugs (e.g., LSD, PCP, etc): These drugs can induce temporary effects that mimic psychosis. However, these symptoms typically cease when the drug wears off. For most people, psychotic symptoms will not be present after first use. It is only after repeated use that psychotic symptoms become more prevalent and long-lasting.
Club/recreational drugs (e.g., ecstasy): Ecstasy can cause psychotic symptoms, antisocial behavior, and panic attacks. Persistent psychosis has been reported after a single use in some people .
How is drug-induced psychosis treated?
Treatment for drug-induced psychosis usually involves stopping the drug that caused the psychosis and then monitoring the person in a safe and calm environment. Therapies and medication can be offered on an inpatient, outpatient or day care basis depending on your circumstances, and may include:
Cognitive behavioural therapy (CBT) – once you have been medically stabilised, the practical and problem-solving talking therapy, Cognitive behavioural therapy, can help you to learn more about the thoughts and moods that you experience before psychotic episodes occur, helping you to manage your emotions and paranoia more readily, and be aware of triggers.
If a mental health condition such as anxiety or depression exists, which has been masked by extensive use of drugs or alcohol to the point of psychosis, then CBT can help you learn techniques to cope with and reduce associated symptoms so as to prevent relapse.
Family therapy – due to the serious nature of drug-induced psychosis and associated psychotic conditions, family therapy involving those closest to you, can help to ensure that there is sufficient support available at home to prevent relapse and manage associated symptoms, potentially reducing the need for extensive hospital treatment.
Anti-psychotic medication – if your underlying mental health condition features psychotic episodes as a symptom, then antidepressant, anti-psychotic or other medications such as clozapine (Clozaril) may be recommended for an extended period of time, particularly if delusions and hallucinations are frequent or particularly severe.