What Is The Safest Drug For Rheumatoid Arthritis?
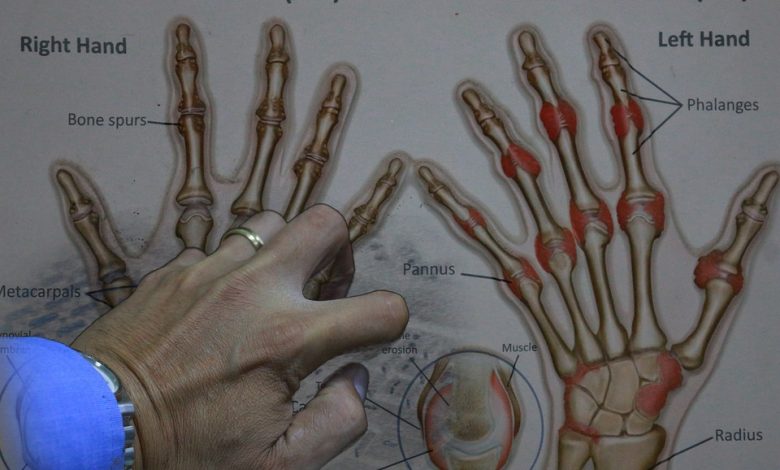
Rheumatoid arthritis (RA) is a chronic autoimmune disorder that causes inflammation, pain, and stiffness in the joints. It affects millions of people worldwide, and it can lead to significant disability if not treated properly.
There are many different drugs available to treat RA, but some are safer than others. In this article, we will discuss the safest drug for rheumatoid arthritis in detail.
Rheumatoid arthritis
Rheumatoid arthritis (RA) is an autoimmune disorder that affects the joints. It is a chronic condition that causes inflammation, pain, and stiffness in the joints. RA affects millions of people worldwide, and it can lead to significant disability if not treated properly. There are many different drugs available to treat RA, but some are safer than others.
The goals of RA treatment are to reduce inflammation, relieve pain, and prevent joint damage. The choice of drugs depends on the severity of the disease, the presence of comorbidities, and the patient’s response to previous treatments. Non-pharmacological treatments such as exercise, physical therapy, and occupational therapy are also important in the management of RA.
Drugs For Rheumatoid Arthritis
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to treat RA. They are effective in reducing pain and inflammation, but they have a risk of gastrointestinal (GI) side effects such as ulcers, bleeding, and perforation. NSAIDs can also increase the risk of cardiovascular events such as heart attack and stroke.
Some NSAIDs are safer than others in terms of GI and cardiovascular risk. For example, selective COX-2 inhibitors such as celecoxib have a lower risk of GI side effects than traditional NSAIDs such as ibuprofen and naproxen. However, COX-2 inhibitors have been associated with an increased risk of cardiovascular events, especially at high doses and in patients with pre-existing cardiovascular disease.
Disease-modifying antirheumatic drugs (DMARDs)
Disease-modifying antirheumatic drugs (DMARDs) are a class of drugs that slow down the progression of RA and prevent joint damage. They are effective in reducing inflammation and improving the quality of life of RA patients. DMARDs can be divided into conventional DMARDs (cDMARDs) and biologic DMARDs (bDMARDs).
cDMARDs include methotrexate, sulfasalazine, leflunomide, and hydroxychloroquine. These drugs have been used for decades in the treatment of RA and have a good safety profile. However, they can cause liver and kidney toxicity, bone marrow suppression, and lung disease in some patients. Regular monitoring of liver and kidney function, blood count, and lung function is recommended for patients taking cDMARDs.
bDMARDs include tumor necrosis factor (TNF) inhibitors such as adalimumab, etanercept, and infliximab, as well as other biologic agents such as rituximab, abatacept, and tocilizumab. These drugs are more targeted and potent than cDMARDs and have revolutionized the treatment of RA in the past two decades. However, they have a higher risk of infections, especially tuberculosis and other opportunistic infections. They can also cause infusion reactions, autoimmune diseases, and malignancies in some patients. Regular monitoring of blood count, liver and kidney function, and immunoglobulin levels is recommended for patients taking bDMARDs.
Janus kinase (JAK) inhibitors
Janus kinase (JAK) inhibitors are a new class of drugs that block the JAK signaling pathway, which is involved in the inflammation and immune response of RA. JAK inhibitors have been approved for the treatment of RA in recent years and have shown promising results in reducing pain and inflammation and preventing joint damage.
There are currently two JAK inhibitors approved for the treatment of RA: tofacitinib and baricitinib. Both drugs have a good safety profile, but they can cause side effects such as infections, liver and kidney toxicity, and blood count abnormalities. Regular monitoring of liver and kidney function, blood count, and cholesterol levels is recommended for patients taking JAK inhibitors.
Glucocorticoids
Glucocorticoids such as prednisone and methylprednisolone are potent anti-inflammatory drugs that are often used to treat RA flares. They can provide rapid relief of symptoms and prevent joint damage, but they have significant side effects if used long-term, such as weight gain, osteoporosis, diabetes, and infections. Therefore, glucocorticoids should be used at the lowest effective dose and for the shortest duration possible.
Conclusion
In conclusion, the safest drug for rheumatoid arthritis depends on various factors such as the severity of the disease, the presence of comorbidities, and the patient’s response to previous treatments. Non-pharmacological treatments such as exercise, physical therapy, and occupational therapy are also important in the management of RA.
NSAIDs are effective in reducing pain and inflammation but have a risk of GI and cardiovascular side effects. Some NSAIDs are safer than others in terms of GI and cardiovascular risk.
cDMARDs have a good safety profile but can cause liver and kidney toxicity, bone marrow suppression, and lung disease in some patients. Regular monitoring of liver and kidney function, blood count, and lung function is recommended for patients taking cDMARDs.
bDMARDs are more targeted and potent than cDMARDs but have a higher risk of infections, infusion reactions, autoimmune diseases, and malignancies. Regular monitoring of blood count, liver and kidney function, and immunoglobulin levels is recommended for patients taking bDMARDs.
JAK inhibitors are a new class of drugs that have a good safety profile but can cause infections, liver and kidney toxicity, and blood count abnormalities. Regular monitoring of liver and kidney function, blood count, and cholesterol levels is recommended for patients taking JAK inhibitors.
Glucocorticoids are potent anti-inflammatory drugs but have significant side effects if used long-term. Therefore, they should be used at the lowest effective dose and for the shortest duration possible.
Overall, the choice of drug for rheumatoid arthritis should be individualized based on the patient’s specific needs and risks. Regular monitoring of side effects and disease activity is essential to ensure the safety and efficacy of RA treatments.





