VIP Peptide and Intestinal Barrier Homeostasis Research
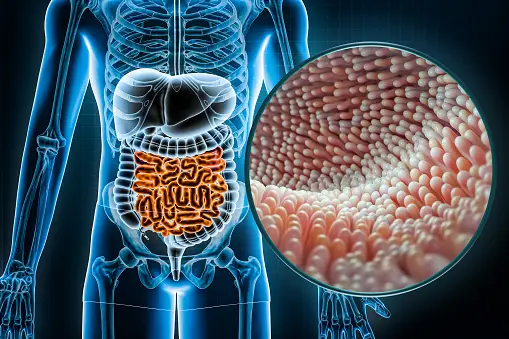
Studies suggest the integrity of the gastrointestinal tract (GIT) may depend on vasoactive intestinal peptide (VIP). VIP is hypothesized to be a powerful anti-inflammatory mediator that may help keep the gastrointestinal tract (GIT) in a steady state by keeping the intestinal epithelial barrier in place, and it might also help keep gut bacteria in check.
Researchers postulated that gut microbial ecology may change if VIP were deficient due to its biological potential. Regardless of gender, the findings implied that VIP-/-mice appeared to have lost weight, have a different bacterial composition, and have a different biodiversity than VIP+/+ and VIP+/-littermates. Consistent with alterations in the gut microbial structure associated with certain inflammatory and autoimmune diseases, VIP-/-mice suggested variations in the makeup of their gut bacteria. According to these findings, VIP appears to be essential for the proper functioning of the gastrointestinal tract (GIT), a major regulator of microbiota diversity and balance, and its genetic deletion might cause a dramatic reorganization of the gut microbiota and subsequent weight loss.
Lelievre et al. (2007) speculated that VIP may control gastric acid production by the stomach, water/ion absorption in the large intestine, peristalsis via regulating smooth muscle contraction, and mucus secretion by Goblet cells inside the gastrointestinal tract. Submucosal and myenteric neutron sources release VIP. VIP has been theorized to keep intestinal epithelial cells (IECs) in good working order, promoting their differentiation, proliferation, and cell adhesion.
Glucagon and leptin are among the six hormones that are metabolically dysregulated in VIP-deficient animals. By producing tolerogenic FoxP3+ Tregs and downregulating co-stimulatory molecules on dendritic cells, VIP in the GIT lamina propria may inhibit inflammation. Research has suggested that VIP knockout mice are more likely to experience chemically induced intestinal inflammation. Similarly, research models with inflammatory bowel disease (IBD) seem to have a decrease in VIP-positive neurons near severely damaged mucosa.
Last but not least, investigations purport that VIP may have mild antibacterial effects against certain commensal bacteria. To sum up, VIP has been speculated to play an important role in immunological tolerance to gut microbiota by providing an anti-inflammatory “tone” and being essential for GIT homeostasis and metabolism. “A deficit in VIPs was suggested to lead to dramatic alterations in biodiversity,” as one report states.
Despite VIP’s biological interactions with the gut microbiota, there is a lack of studies outlining the impact of VIP signaling on microbial ecology. One research study suggested that pig gut bacterial composition appeared to have changed after receiving VIP and reduced diarrhea and weight loss in a model of bacterial illness.
VIP Peptide and the Digestive Tract
Findings imply that neuropeptides like gastrin-releasing peptide (GRP) and vasoactive intestinal peptide (VIP) may impact the cephalic phase, and the exocrine pancreas possesses peptidergic nerve terminals that might explain this. Furthermore, muscarinic and VIP receptors are speculated to be involved in the mechanism by which thyrotropin-releasing hormone may induce the exocrine production of bicarbonate and protein from the pancreas via vagal afferents.
Researchers have indicated that infusing dogs with bovine bile and bile acids might stimulate the production of many hormones and neuropeptides, including secretin, CCK, neurotensin, VIP, GIP, PP, and somatostatin. Increased fluid and bicarbonate release in response to higher VIP plasma levels provides further speculation that bile stimulates peptidergic neurons, triggering pancreatic secretion. Because atropine inhibits the exocrine pancreatic production of bile and taurocholate, cholinergic processes are also crucial.
Compared to TDC, the impact of bile appeared to be somewhat greater. A notable rise in plasma VIP and SLI concentrations was hypothesized to occur concurrently with the pancreatic response. There seems to be a concentration-dependent relationship between bile and the concentrations of integrated plasma VIP and SLI… Thus, VIP may be an additional intermediary between bicarbonate production and bile volume.
When it comes to potentially stimulating pancreatic secretion, Vasoactive intestinal peptide and secretin are compared. The highest bicarbonate production in response to VIP seemed only around 17% of that to secretin, and prior research in dogs indicated that VIP appeared to be a far weaker pancreatic secretion stimulant than secretin. VIP is believed to activate pancreatic bicarbonate secretion in cats fully but only partially in dogs. Thirdly, findings implied that secretin and VIP appeared to be equally effective in cats, and when combined, they seemed to have enhanced pancreatic bicarbonate secretion with additive kinetics. In contrast, VIP was determined to be less effective than secretin and to inhibit pancreatic secretion that was secretin-induced competitively in dogs.
VIP Peptide and Insulin
In addition to the neurotransmitter acetylcholine, there are at least two other neuropeptides found in islet parasympathetic nerve endings that may play a role in stimulating insulin secretion: pituitary adenylate cyclase-activating polypeptide (PACAP) and vasoactive intestinal peptide (VIP). PACAP, VIP’s parent, also seems to regulate the production of other components.
VIP Peptide and the Intestinal Barrier
When it comes to colitis caused by Citrobacter rodentium, Vasoactive intestinal peptide has been theorized to help restore the intestinal barrier.
Permeability increases, and luminal contents may reach the underlying milieu when bacterial infections, either adhering to or effacing from the apical surface of epithelial cells, compromise the function of the epithelial barrier.
The neuropeptide Vasoactive intestinal peptide (VIP) has been speculated to modulate epithelial paracellular permeability in previous in vitro experiments. This activity would be supported by the high concentrations and proximity of VIP-containing nerve fibers to intestinal epithelial cells.
Click here if you are a researcher interested in further studying the potential of VIP peptides.
References
[i] Bains, Manpreet, et al. “Vasoactive Intestinal Peptide Deficiency Is Associated with Altered Gut Microbiota Communities in Male and Female C57BL/6 Mice.” Frontiers in Microbiology, vol. 10, 2 Dec. 2019, 10.3389/fmicb.2019.02689. [ii] Wikipedia Contributors. “Vasoactive Intestinal Peptide.” Wikipedia, Wikimedia Foundation, 22 Oct. 2019, en.wikipedia.org/wiki/Vasoactive_intestinal_peptide [iii] “Regulation of Pancreatic Secretion.” The Pancreapedia: Exocrine Pancreas Knowledge Base, 2019, https://www.pancreapedia.org/reviews/regulation-of-pancreatic-secretion-version-10, 10.3998/panc.2015.38. [iv] Riepl, R. L., et al. “Effect of Intraduodenal Bile and Taurodeoxycholate on Exocrine Pancreatic Secretion and on Plasma Levels of Vasoactive Intestinal Polypeptide and Somatostatin in Man.” Pancreas, vol. 9, no. 1, 1 Jan. 1994, pp. 109–116, pubmed.ncbi.nlm.nih.gov/7509061/, 10.1097/00006676-199401000-00016. [v] Konturek, S. J., et al. “Comparison of Vasoactive Intestinal Peptide and Secretin in Stimulation of Pancreatic Secretion.” The Journal of Physiology, vol. 255, no. 2, 1 Feb. 1976, pp. 497–509, pubmed.ncbi.nlm.nih.gov/1255530/, 10.1113/jphysiol.1976.sp011292. [vi] Conlin, V. S., et al. “Vasoactive Intestinal Peptide Ameliorates Intestinal Barrier Disruption Associated with Citrobacter Rodentium-Induced Colitis.” American Journal of Physiology-Gastrointestinal and Liver Physiology, vol. 297, no. 4, Oct. 2009, pp. G735–G750, 10.1152/ajpgi.90551.2008. [vii] Keita, Å. V., et al. “Vasoactive Intestinal Polypeptide Regulates Barrier Function via Mast Cells in Human Intestinal Follicle-Associated Epithelium and during Stress in Rats.” Neurogastroenterology& Motility, vol. 25, no. 6, 18 Apr. 2013, pp. e406–e417, 10.1111/nmo.12127. [viii] Wu, Xiujuan, et al. “Vasoactive Intestinal Polypeptide Promotes Intestinal Barrier Homeostasis and Protection against Colitis in Mice.” PLoS ONE, vol. 10, no. 5, 1 May 2015, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4416880/, 10.1371/journal.pone.0125225.