List of Drugs that Can Cause Purpura

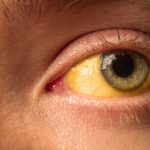
Purpura is a medical term used to describe purple or red discolorations on the skin due to bleeding underneath the skin’s surface. It can result from various underlying causes, including drug reactions. While purpura caused by drugs is relatively rare, it is essential to be aware of the medications that can lead to this condition.
This article aims to provide a comprehensive list of drugs that have been associated with purpura and some insights into the mechanisms behind these drug-induced skin reactions.
Understanding Purpura
Before delving into the list of drugs, it’s vital to understand what purpura is and how it occurs. Purpura refers to pinpoint bleeding underneath the skin, leading to the characteristic purple or red spots. These spots can vary in size and may be associated with pain or itching. Purpura can be caused by a variety of factors, including trauma, infections, blood disorders, and medications.
Drugs and Purpura
When a drug triggers purpura, it typically falls into one of two categories: those that cause a direct toxic effect on blood vessels and those that affect blood clotting. Some drugs can cause purpura by inducing vasculitis, an inflammation of the blood vessels. Others may lead to purpura by altering platelet function or other components of the clotting cascade.
Drug-induced purpura can arise from a variety of medications and is characterized by the development of purple or red discolorations on the skin due to bleeding beneath the skin’s surface. Understanding the connection between these drugs and purpura is crucial, as early recognition can lead to better management and potentially the discontinuation of the medication in question.
List of Drugs Associated with Purpura
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Certain NSAIDs, such as aspirin and ibuprofen, have been occasionally linked to the development of purpura. Although the precise mechanism remains unclear, it is believed to be related to their effects on platelet function and the potential for causing inflammation of blood vessels. These drugs are commonly used for pain relief and reducing inflammation, but in rare cases, they may trigger this unwanted side effect.
- Anticoagulants: Anticoagulant medications, including heparin and warfarin, are prescribed to prevent the formation of blood clots. However, these drugs can sometimes result in bleeding disorders and purpura. The risk of purpura with anticoagulants is associated with their inherent property of inhibiting blood clot formation, which can occasionally lead to unwanted bleeding in the skin’s layers
- Thrombolytic Agents: Thrombolytics like alteplase and streptokinase are used to dissolve blood clots, especially in life-threatening situations such as heart attacks and strokes. While these drugs are indispensable for emergency medical interventions, they come with an increased risk of bleeding, including purpura, due to their capacity to break down blood clots in the circulatory system.
- Platelet Aggregation Inhibitors: Medications that inhibit platelet aggregation, such as clopidogrel and ticlopidine, may lead to the development of purpura. These drugs hinder the ability of platelets to clump together and form clots. In some instances, this can result in a higher susceptibility to bleeding, including the appearance of purpura.
- Certain Antibiotics: Certain antibiotics, such as penicillin, cephalosporins, and sulfonamides, have been associated with purpura in specific cases. The exact cause of this side effect isn’t fully understood, but it may be related to allergic reactions or immune-mediated responses to the antibiotics.
- Immunosuppressive Drugs: Immunosuppressive medications like azathioprine and cyclosporine, which are often prescribed to organ transplant recipients to prevent organ rejection, can weaken the immune system’s response. This immunosuppression may lead to various skin manifestations, including purpura, in susceptible individuals.
- Angiotensin-Converting Enzyme (ACE) Inhibitors: ACE inhibitors are commonly used to treat hypertension and heart conditions. While the exact mechanism behind their association with purpura is not entirely clear, they have been reported to cause purpura in rare instances. This side effect serves as a reminder for healthcare professionals to monitor patients closely when using ACE inhibitors.
- Antipsychotic Medications: Some antipsychotic drugs, particularly older-generation drugs like chlorpromazine, have been linked to skin reactions, including purpura. The occurrence of purpura in these cases is often one of several side effects associated with these medications.
- Antiplatelet Drugs: Medications like aspirin, dipyridamole, and cilostazol are used to reduce platelet aggregation and, thereby, prevent blood clot formation. However, their anticoagulant effects can sometimes lead to purpura in individuals who may be more sensitive to these drugs or with underlying bleeding tendencies.
- Chemotherapeutic Agents: Various chemotherapy drugs, such as specific alkylating agents and tyrosine kinase inhibitors, can lead to purpura as a side effect. This is primarily due to their impact on blood cells and the body’s overall physiology during cancer treatment. The presence of purpura may be one of several adverse effects associated with chemotherapy.
Mechanisms and Risk Factors
The mechanisms behind drug-induced purpura can vary, but they often involve changes in platelet function, clotting factors, or blood vessel inflammation. Factors that may increase the risk of developing purpura with these drugs include:
- Individual sensitivity or allergy to the medication.
- High doses or prolonged use of the drug.
- Interaction with other medications.
- Underlying medical conditions that affect blood clotting or blood vessel health.
Prevention and Management
Preventing drug-induced purpura primarily involves awareness and cautious use of medications. Healthcare providers should be diligent in monitoring patients for potential side effects, including skin reactions when prescribing these drugs. If purpura develops, discontinuing the medication and seeking medical attention are essential steps. In some cases, alternative medications may be considered.
Conclusion
While drug-induced purpura is relatively rare, it is crucial to be aware of the medications that can potentially cause this condition. Patients and healthcare providers should maintain open communication and exercise caution when using drugs known to be associated with purpura. Early recognition and appropriate management are key to minimizing the impact of this skin condition and ensuring patient safety. It is essential to consult a healthcare professional for a proper diagnosis and guidance on treatment when any unusual skin reactions occur while taking medication.