List of Drugs That Can Cause Hypocalcemia

Hypocalcemia is a medical condition characterized by lower-than-normal levels of calcium in the blood. Calcium is an essential mineral that plays a crucial role in various physiological functions within the human body. It is vital for the formation and maintenance of strong bones and teeth, blood clotting, muscle contraction, nerve function, and various enzymatic processes.
The normal range of calcium in the blood is typically between 8.5 to 10.2 milligrams per deciliter (mg/dL). Hypocalcemia occurs when the calcium levels fall below this normal range, leading to disruptions in the body’s normal functioning.
The symptoms of drug-induced hypocalcemia can vary in severity and may include:
1. Muscle Cramps and Spasms: Calcium is essential for normal muscle contraction. A lack of calcium can result in muscle cramps, spasms, and tetany (prolonged muscle contractions).
2. Tingling or Numbness: Hypocalcemia can cause tingling or numbness, especially around the mouth and in the extremities.
3. Seizures: Low calcium levels can increase the excitability of nerve cells, potentially leading to seizures.
4. Mood Changes: Calcium plays a role in neurotransmitter release, and hypocalcemia may be associated with irritability, anxiety, or depression.
5. Cardiac Abnormalities: Severe hypocalcemia can affect the electrical conduction system of the heart, leading to arrhythmias and other cardiac complications.
Hypocalcemia can result from various factors, including medications. Calcium is an essential mineral vital for numerous physiological functions within the human body, including bone formation, muscle contraction, and blood clotting. Certain drugs, whether prescribed or over-the-counter, may interfere with calcium metabolism, leading to hypocalcemia. In this article, we will delve into a comprehensive list of drugs known to be associated with hypocalcemia, exploring their mechanisms of action and potential consequences.
List of Drugs That Can Cause Hypocalcemia
The list of drugs that can cause hypocalcemia include:
1. Proton Pump Inhibitors (PPIs)
Proton pump inhibitors, commonly used to treat conditions like gastroesophageal reflux disease (GERD) and peptic ulcers, have been linked to hypocalcemia. These drugs, including omeprazole, esomeprazole, and lansoprazole, can hinder the absorption of calcium from the gastrointestinal tract, contributing to reduced serum calcium levels.
2. Loop Diuretics
Loop diuretics, such as furosemide and bumetanide, are medications prescribed to manage conditions like edema and hypertension. These drugs act on the kidneys, promoting the excretion of water and electrolytes, including calcium. Excessive use of loop diuretics can lead to increased urinary calcium loss, resulting in hypocalcemia.
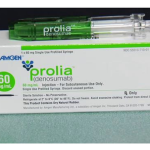
3. Bisphosphonates
Bisphosphonates, a class of drugs frequently prescribed for the treatment of osteoporosis and other bone-related disorders, can interfere with calcium metabolism. These medications, which include alendronate and risedronate, may disrupt the balance between bone resorption and formation, potentially causing a decrease in serum calcium levels.
4. Antiepileptic Drugs
Certain antiepileptic drugs, such as phenytoin and phenobarbital, have been associated with hypocalcemia. These medications can affect the metabolism of vitamin D, a crucial regulator of calcium absorption. Additionally, they may interfere with calcium-binding proteins, further contributing to decreased calcium levels.
5. Aminoglycoside Antibiotics
Aminoglycoside antibiotics, including gentamicin and tobramycin, are known for their potent antimicrobial properties. However, these drugs can have adverse effects on calcium homeostasis by impairing renal function and promoting renal calcium excretion, potentially leading to hypocalcemia.
6. Corticosteroids
Corticosteroids, commonly prescribed for their anti-inflammatory and immunosuppressive effects, may impact calcium metabolism. These drugs can inhibit calcium absorption in the intestines, increase renal calcium excretion, and influence bone turnover, collectively contributing to hypocalcemia.
7. Antifungal Azoles
Certain antifungal medications, such as ketoconazole and itraconazole, have been associated with hypocalcemia. These drugs can interfere with vitamin D metabolism and inhibit the activity of calcium channels, contributing to decreased calcium absorption and utilization.
8. Chemotherapy Agents
Some chemotherapy agents, particularly those used in the treatment of malignancies, can contribute to hypocalcemia. Cisplatin and certain tyrosine kinase inhibitors may impact calcium homeostasis through various mechanisms, including renal dysfunction and interference with vitamin D metabolism.
Coping with Drug-Induced Hypocalcemia
Hypocalcemia, characterized by abnormally low levels of calcium in the blood, can be induced by certain medications. Coping with drug-induced hypocalcemia involves a combination of medical management, lifestyle adjustments, and ongoing communication with healthcare professionals.
Consult Your Healthcare Provider
If you suspect or have been diagnosed with drug-induced hypocalcemia, it’s crucial to consult your healthcare provider immediately. Provide a detailed medical history, including a list of medications you are currently taking, to help the healthcare provider identify the potential cause of hypocalcemia.
Adjust Medications
If a specific medication is identified as the cause of hypocalcemia, your healthcare provider may consider adjusting the dosage, changing the medication, or prescribing an alternative. Never adjust your medications without consulting your healthcare provider.
Calcium Supplementation
In some cases, your healthcare provider may prescribe calcium supplements to raise and maintain blood calcium levels. Calcium supplements may come in various forms, including calcium carbonate and calcium citrate. Follow your healthcare provider’s recommendations regarding the type and dosage of calcium supplements.
Vitamin D Supplementation
Vitamin D is essential for calcium absorption. If hypocalcemia is related to vitamin D deficiency, your healthcare provider may prescribe vitamin D supplements. Adequate exposure to sunlight can also help the body produce vitamin D naturally.
Regular Monitoring
Regular monitoring of blood calcium levels is crucial to assess the effectiveness of treatment and make adjustments as needed. Follow-up appointments with your healthcare provider are essential to track your progress and address any emerging issues.
Dietary Changes
Maintain a diet rich in calcium-containing foods, such as dairy products, green leafy vegetables, and fortified foods. Limit the intake of substances that can interfere with calcium absorption, such as excessive caffeine and alcohol.
Stay Hydrated
Ensure adequate hydration, as dehydration can exacerbate the symptoms of hypocalcemia.
Exercise and Physical Therapy
Engage in regular, moderate exercise to support bone health and overall well-being. If muscle spasms or weakness are present, physical therapy may be beneficial to improve muscle strength and function.
Education and Support
Educate yourself about drug-induced hypocalcemia, its causes, and management strategies. Seek support from healthcare professionals, support groups, or organizations specializing in conditions related to calcium metabolism.
Emergency Preparedness
Be aware of the signs and symptoms of severe hypocalcemia, such as seizures or cardiac abnormalities. Have a plan in place for emergencies, including knowing when to seek immediate medical attention.
Always follow the guidance of your healthcare provider, and do not make significant changes to your treatment plan without consulting them. Open communication and a collaborative approach with your healthcare team are essential for effectively managing drug-induced hypocalcemia.