How to Decode a Doctor’s Hand Written Prescription

It is generally accepted that doctors have illegible handwriting. The writer usually knows what is written, but other parties often have problems with reading and interpreting. Reading a doctor’s handwritten prescription can feel like trying to understand a foreign language. Between confusing pharmacy abbreviations, complicated medical names and other bits of information, it’s natural for your eyes to glaze over after just a few seconds. Whether you’re a prospective pharmacy technology student looking to better understand the prescription process or a consumer trying to decode what your doctor writes on your prescription, this educational guide easily breaks down how prescriptions work.
Despite their confusing nature, medication labels contain important information about a prescription, so it’s necessary to have at least a fundamental grasp on what it all means. Remember, you can always ask your pharmacist or pharmacy technician to clarify anything you don’t understand.
Who Can Write Prescriptions?
Both federal and local laws give a wide range of different medical professionals the ability to write prescriptions. Physicians, physician assistants, advanced practice registered nurses, nurse practitioners, anesthetists, certified nurse midwives and clinical nurse specialists currently have the power to do so in all fifty states. In some states, clinical pharmacists can write prescriptions, as long as it is in collaboration with a physician or drug formulary.
Why Is It Important To Know My Prescription?
Understanding exactly what your prescription means is invaluable for a few different reasons. For starters, being clear on which medications you should take and which you should avoid can help you evade adverse drug reactions, which can occur when taking multiple medications. There are two million serious adverse drug reactions (also called ADRs) per year, which results in over 100,000 deaths. 82% of American adults take at least one medication, and 29% of all patients in the United States take more than five medications at a time. To put this into perspective, the rate of an ADR increases exponentially when patients take more than four medications.
Common adverse drug reactions caused by drug interactions
• Aspirin and Warfarin, when taken together, increase your risk of bleeding.
• Lithium and Diuretics can alter the levels of sodium in your kidneys.
• Oral contraceptives and rifampin, an antibiotic, can cause contraceptives to be less effective when taken at the same time.
What Goes Into A Prescription?
A standard medical prescription usually includes a few key pieces of information like the name of the drug, the strength and the recommended dosage. It will also include specific directions for how you should use it, the total quantity of the medication that is being prescribed and the number of authorized refills that you have before the prescription will need to be renewed.
What Do Those Prescription Abbreviations Mean?
The pharmaceutical abbreviations that physicians use are often based on a combination of Latin and prescription shorthand, designed to get important information across as quickly as possible, to save space and to make it more difficult for a patient to alter a prescription on their own. These medication abbreviations are broken down into a few different categories:
Medical Abbreviations That Indicate When To Take Your Medication:
• AC, from the Latin 1 “ante cibum,” means “take before a meal.”
• HS, from the Latin “hora somni,” means “take at bedtime.”
• PC, from the Latin “post cibum,” means “take after a meal.”
Medical Abbreviations That Describe How To Use Your Medication:
• PO, from the Latin “per os,” or “by mouth,” means that medication should be taken orally.
• AD, from the Latin “auris dexter,” or “right ear,” means that your medication should be taken via your right ear.
• AS, from the Latin “auris sinister,” or “left ear,” means that your medication should be taken via your left year.
• AU, from the Latin “auris utro” or “each ear,” denotes medication meant to be taken in both ears.
• OD, from the Latin “oculus dexter,” or “right eye,” and OS, from the Latin “oculus sinister,” or “left eye,” mean that medication is for your right eye or left eye, respectively.
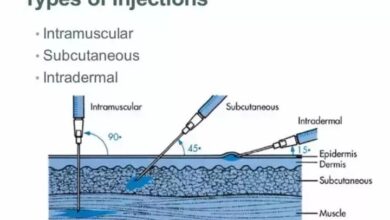
• SUBQ indicates that medication should be taken subcutaneously.
• SUP means that medication is a suppository.
Medical Abbreviations That Inform How Often to Take Your Medication:
• BID, from the Latin “bis in die,” means that the medication should be taken “twice a day.”
• PRN, from the Latin “pro re nata,” means that the medication should be taken “as needed.”
• Q, from the Latin “quaque,” means “every,” with medical abbreviations like QHR meaning every hour, Q4HR meaning every four hours, etc.
Dosage Information:
• i, ii, iii and iiii medical abbreviations indicate dose size and equate to 1, 2, 3 and 4.
What About Generic Drugs?
According to the Food and Drug Administration, a generic drug is one that is comparable to a brand name medication in form, strength, route of administration, quality and more. Generic drugs are often 80 to 85% less expensive than their brand name counterparts. As a result, 80% of all prescriptions filled in the United States are for these generic medications.