Qiliqiangxin and Heart failure With Reduced Ejection Fraction (HFrEF)
Heart failure with reduced ejection fraction (HFrEF) is a type of heart failure where the heart’s ability to pump blood is impaired, resulting in a reduced ejection fraction. The ejection fraction is a measurement of the percentage of blood pumped out of the heart’s left ventricle with each heartbeat.
In HFrEF, the heart’s left ventricle doesn’t contract as effectively as it should, which leads to a decreased ability to pump a sufficient amount of blood to meet the body’s needs. This can result in symptoms such as fatigue, shortness of breath, fluid retention (edema), and exercise intolerance. HFrEF is often associated with structural changes in the heart, such as enlargement of the left ventricle and weakening of the heart muscle.
Treatment for HFrEF typically focuses on improving symptoms, enhancing quality of life, and prolonging survival. Common treatment approaches may include:
1. Medications: There are several classes of medications used to manage HFrEF, including angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), beta-blockers, and mineralocorticoid receptor antagonists. These medications can help reduce symptoms, improve heart function, and prevent further deterioration of the heart.
2. Lifestyle Changes: Lifestyle modifications such as reducing salt intake, managing fluid intake, and maintaining a healthy weight are important to manage fluid retention and overall heart health.
3. Exercise: Regular, controlled exercise can improve heart function, enhance exercise tolerance, and boost overall well-being. However, exercise plans should be tailored to individual capabilities and discussed with a healthcare provider.
4. Diet: A heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats is recommended. This can help manage conditions like hypertension and diabetes that often contribute to heart failure.
5. Implantable Devices: Some individuals with HFrEF may benefit from implantable devices such as cardiac resynchronization therapy (CRT) devices or implantable cardioverter-defibrillators (ICDs) to improve heart function and prevent life-threatening arrhythmias.
6. Surgical Interventions: In certain cases, surgical procedures like coronary artery bypass grafting (CABG) or heart valve repair/replacement may be necessary to address underlying causes of HFrEF.
Management of HFrEF requires a comprehensive and individualized approach. Regular monitoring, adherence to medical recommendations, and open communication with healthcare providers are essential for effective management and improved quality of life for individuals with this condition.
What is Qiliqiangxin?
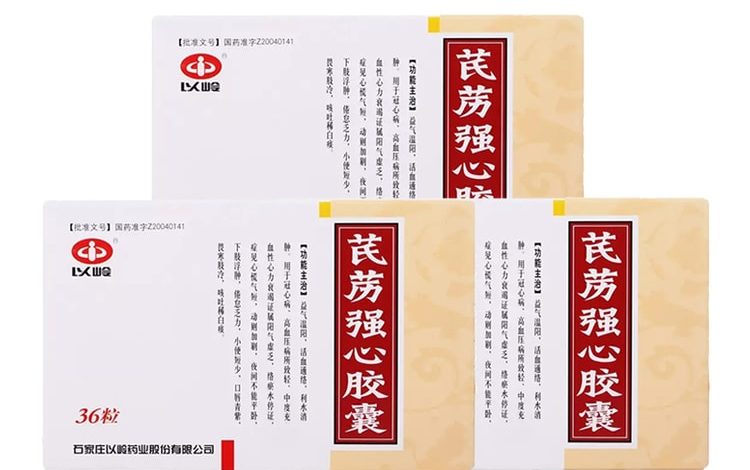
Qiliqiangxin (also known as Qili Qiangxin or QLQX) is a traditional Chinese herbal medicine that has been developed and used for the treatment of heart failure. It’s a complex herbal formula that combines multiple herbs with the aim of improving heart function and managing symptoms associated with heart failure. The formula is based on principles from Traditional Chinese Medicine (TCM) and has been studied for its potential benefits in heart failure management, particularly in heart failure with reduced ejection fraction (HFrEF).
Qiliqiangxin is believed to work through a combination of mechanisms, including improving cardiac contractility, enhancing blood circulation, and reducing inflammation. Some studies suggest that it might have a positive impact on symptoms, exercise tolerance, and overall quality of life in individuals with heart failure.
A recent large placebo-controlled trial presented at the European Society of Cardiology (ESC) 2023 Congress investigated the effects of the traditional Chinese medicine Qiliqiangxin (QLQX) on heart failure with reduced ejection fraction (HFrEF) when combined with guideline-directed therapies. Qiliqiangxin is composed of 11 plant-based substances known for diuretic effects, vasodilation, and potential heart-supporting properties. The trial, known as QUEST, enrolled patients with HFrEF receiving an optimized triple-therapy regimen and aimed to assess whether Qiliqiangxin could reduce cardiovascular death and heart failure hospitalization compared to placebo.
Results showed that Qiliqiangxin, when added to standard treatments, led to a significant reduction of more than 20% in the composite endpoint of cardiovascular death and heart failure hospitalization. The risk reductions were consistent across various patient subgroups and both endpoints. The treatment was generally well-tolerated. Notably, the benefits of Qiliqiangxin appeared to overlap with those of guideline-directed therapies, with a trend of greater benefit in patients not receiving the complete triple therapy. While these findings support Qiliqiangxin’s potential clinical benefit, further studies are needed to explore its mechanisms of action and optimal use in the management of HFrEF.
It’s important to note that while Qiliqiangxin has shown promise in certain clinical studies, it is not a standard treatment option for heart failure in many countries, and its use may be limited to specific regions or under the guidance of qualified practitioners familiar with TCM.
If you or someone you know is considering using Qiliqiangxin for heart failure management, it’s crucial to consult with a healthcare professional, preferably one with expertise in both conventional cardiology and traditional medicine. This is important to ensure that the treatment approach is safe, appropriate, and well-coordinated with any other medical interventions or medications that may be in place.





