Intrathecal Drug Delivery: Benefits and Associated Risks

What does the medical term intrathecal mean?
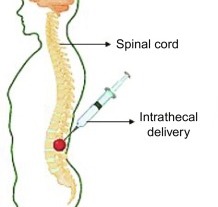
The term “Intrathecal” refers to a medical procedure or administration route that involves the introduction of substances into the space surrounding the spinal cord known as the intrathecal space. The term “intrathecal” comes from the Latin words “intra,” meaning “within,” and “theca,” meaning “sheath” or “covering.”
Intrathecal administration typically involves injecting medications or other substances directly into the intrathecal space, where cerebrospinal fluid circulates. This route allows for direct access to the central nervous system, bypassing the blood-brain barrier, which can be advantageous in certain medical situations.
Common applications of intrathecal administration include:
1. Pain management: Medications such as opioids or local anesthetics can be delivered intrathecally to provide targeted pain relief, especially in cases of chronic pain or cancer-related pain.
2. Chemotherapy: Some cancer treatments involve delivering chemotherapy drugs directly into the cerebrospinal fluid via intrathecal administration. This method can be used to treat or prevent the spread of cancer cells to the central nervous system.
3. Diagnostic procedures: Intrathecal injections of contrast agents or radioactive tracers can help visualize the spinal cord and surrounding structures during certain diagnostic tests, such as myelograms or cisternograms.
It’s important to note that intrathecal administration should be performed by trained medical professionals in a controlled setting due to its invasive nature and potential risks.
Intrathecal Drugs
Intrathecal drugs are medications or substances administered directly into the intrathecal space surrounding the spinal cord, allowing them to bypass the blood-brain barrier and reach the central nervous system. Here is a list of 20 commonly used drugs for intrathecal administration:
1. Morphine: An opioid analgesic used for pain management in conditions such as cancer or chronic pain.
2. Baclofen: A muscle relaxant used to treat spasticity caused by conditions like multiple sclerosis or spinal cord injury.
3. Methotrexate: A chemotherapy drug used intrathecally to treat or prevent cancer cells from spreading to the central nervous system.
4. Cytarabine (ara-C): Another chemotherapy agent used intrathecally to treat leukemia or lymphoma that affects the central nervous system.
5. Hydrocortisone: A corticosteroid used to reduce inflammation and treat conditions like spinal cord injury or certain autoimmune disorders.
6. Bupivacaine: A local anesthetic used for pain relief during surgery or in chronic pain management.
7. Fentanyl: A potent opioid analgesic used for severe pain management, especially in cancer patients.
8. Clonidine: A medication primarily used for managing high blood pressure but also employed for intrathecal pain management.
9. Glycerin: Used intrathecally to treat conditions like trigeminal neuralgia or chronic pain.
10. Ziconotide: A synthetic peptide used for the management of severe chronic pain, particularly in cases refractory to other treatments.
11. Tetracaine: A local anesthetic used for spinal or epidural anesthesia and analgesia.
12. Lioresal Intrathecal (Baclofen): An intrathecal formulation of baclofen used for the treatment of severe spasticity.
13. Gabapentin: A medication used to manage neuropathic pain and seizures that may also be administered intrathecally.
14. Meperidine (Pethidine): An opioid analgesic used for moderate to severe pain relief.
15. Lidocaine: A local anesthetic employed for spinal anesthesia or pain management.
16. Busulfan: A chemotherapy drug sometimes used intrathecally as part of stem cell transplantation protocols.
17. Etoposide: A chemotherapy medication used intrathecally in the treatment of certain cancers, including leukemia.
18. Tenecteplase: A thrombolytic agent used intrathecally in some cases of acute ischemic stroke.
19. Carboplatin: A platinum-based chemotherapy drug sometimes administered intrathecally to treat certain cancers.
20. Ara-C (Cytarabine): A chemotherapy drug used intrathecally for the treatment of lymphomas and leukemia.
Please note that this is not an exhaustive list, and the use of intrathecal drugs should be determined by healthcare professionals based on individual patient needs and specific medical conditions.

Risks Associated With Intrathecal Administration Of Drugs
Intrathecal administration of drugs carries certain risks and potential complications, which should be considered before undergoing the procedure. Some of the common risks associated with intrathecal drug administration include:
1. Infection: Any invasive procedure carries a risk of infection. In the case of intrathecal administration, there is a potential risk of introducing bacteria or other pathogens into the spinal region, leading to meningitis or other infections.
2. Bleeding: There is a small risk of bleeding at the injection site or in the spinal region. This risk may be higher for individuals with bleeding disorders or those taking anticoagulant medications.
3. Nerve damage: Improper needle placement or accidental damage to nerves within the spinal region can result in nerve injury. This can lead to symptoms such as numbness, weakness, or pain.
4. Allergic reactions: Some individuals may be allergic to the medications or substances used in intrathecal administration. Allergic reactions can range from mild to severe, including anaphylaxis, a potentially life-threatening allergic response.
5. Cerebrospinal fluid leak: The injection site may inadvertently cause a cerebrospinal fluid leak, which can lead to complications such as headaches, dizziness, or infection.
6. Side effects of the medication: The drugs administered intrathecally may have their own side effects, including nausea, dizziness, respiratory depression, or sedation.
7. Incorrect dosage or drug interactions: Errors in dosage calculations or drug interactions can occur, leading to inadequate pain relief or adverse effects.
It’s essential to discuss these risks with a healthcare professional before undergoing intrathecal drug administration. The procedure should only be performed by trained medical personnel in a controlled environment to minimize potential risks and ensure patient safety.
What is the difference between an epidural and an intrathecal?
Both epidural and intrathecal procedures involve the administration of medications or substances in the spinal region; however, there are key differences between the two methods.
An epidural refers to the placement of a catheter in the epidural space, which is the outermost space surrounding the spinal cord and the protective covering called the dura mater. Epidural administration is commonly used for pain relief during childbirth, surgery, or chronic pain management. Medications, such as local anesthetics or opioids, are delivered into the epidural space to target nerve roots and provide pain relief in a specific region of the body. The effects of epidural administration are typically localized, and the medication may spread to nearby nerve roots and the bloodstream to a limited extent.
On the other hand, intrathecal administration involves the injection of medications or substances directly into the intrathecal space, which is the space within the dura mater and surrounds the spinal cord. By bypassing the blood-brain barrier, intrathecal delivery allows for direct access to the central nervous system. This method is often used for targeted pain management, such as in cases of chronic pain or cancer-related pain, and for administering certain chemotherapy drugs to treat or prevent cancer cells from spreading to the central nervous system. Intrathecal administration typically results in a more concentrated effect on the central nervous system than epidural administration.