Does the Second Dose of Sutab Work Faster?
Sutab is a medication commonly prescribed for bowel preparation before diagnostic procedures like colonoscopies. The effectiveness and efficiency of this medication are crucial for successful and accurate medical examinations.
Patients often wonder whether the second dose of Sutab works faster than the initial one, as the timing and efficacy of each dose can impact the overall experience and success of the procedure.
What is Sutab?
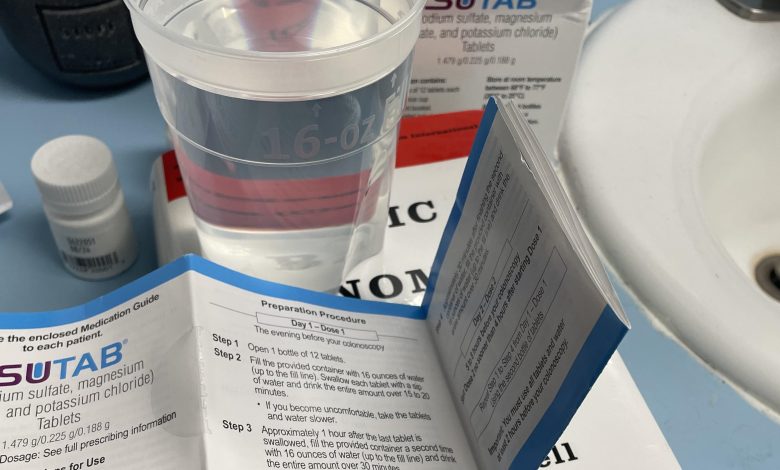
Sutab is a combination of three medications – sodium sulfate, potassium sulfate, and magnesium sulfate. These ingredients work together as an osmotic laxative to induce diarrhea, effectively cleansing the colon before medical imaging or surgery. Proper bowel preparation is essential for clear visualization of the colon and accurate diagnosis during procedures like colonoscopies.
Understanding the Two-Dose Regimen
The standard bowel preparation procedure with Sutab typically involves two doses taken before the scheduled medical procedure. Patients are usually instructed to take the first dose on the evening before the procedure, followed by the second dose on the morning of the examination.
Does the Second Dose Work Faster?
While there might be a perception that the second dose of Sutab could work faster due to a cumulative effect, the reality is that the timing and efficacy of each dose are carefully calibrated to optimize colon cleansing. The two-dose regimen is designed to ensure a thorough and effective bowel preparation process, minimizing the risk of complications during the medical procedure.
The first dose of Sutab initiates the process of clearing the colon, and the second dose acts as a reinforcement to complete the cleansing. The interval between the two doses is strategically determined to allow sufficient time for the medication to take effect without compromising the patient’s safety.
Factors Influencing Bowel Preparation
Several factors can influence the effectiveness and speed of bowel preparation with Sutab, and these should be considered when assessing the overall experience:
1. Patient Compliance: Adhering to the prescribed dosing schedule is crucial. Missing doses or altering the timing can compromise the effectiveness of bowel preparation.
2. Individual Variability: The response to medications can vary among individuals. Factors such as metabolism and overall health can influence how quickly the body responds to Sutab.
3. Dietary Restrictions: Following dietary guidelines provided by healthcare professionals is essential. Certain foods may interfere with the effectiveness of the medication.
4. Hydration: Staying adequately hydrated is important during the bowel preparation process. Dehydration can impact the efficacy of Sutab and the overall experience for the patient.
Conclusion
In conclusion, the second dose of Sutab is not designed to work faster but rather to complement the first dose in achieving optimal bowel preparation. Patient compliance, adherence to dietary guidelines, and proper hydration play significant roles in the success of the bowel preparation process. It is essential for individuals undergoing medical procedures to follow their healthcare provider’s instructions meticulously to ensure a safe and effective experience. If there are any concerns or questions about the medication, patients should consult their healthcare professionals for personalized guidance.





