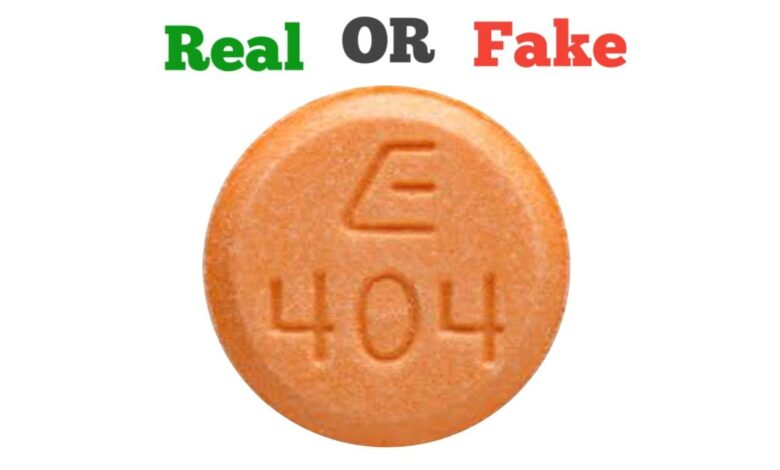
How to Spot Fake E 404 Pill
The round, orange pill with the imprint E 404 has been identified as Amphetamine and Dextroamphetamine 30 mg (Adderall) supplied by Sandoz Pharmaceuticals Inc.. Amphetamine and dextroamphetamine combination like E 404 pill is used to treat attention-deficit hyperactivity disorder (ADHD) and narcolepsy (uncontrollable desire for sleep or sudden attacks of deep sleep). These two medicines belong to the group of medicines called central nervous system (CNS) stimulants.
Recently, health officials issued a warning that drug dealers are selling dangerous drugs that look like prescription medication. Law enforcement officials said the phony pills could pose a danger to young people who take prescription drugs that aren’t their own. “The biggest trend we’ve seen is methamphetamine being pressed into a pill form as Adderall,” said Richard Sawyer, chief deputy of the Rockingham County Sheriff’s Office. “Adderall is a drug that is commonly used for attention deficit disorder.”
The Department of Justice also announced that it has arrested a Worcester man for possession with intent to distribute methamphetamine disguised as counterfeit Adderall pills. Nestiano Kristo, 20, of Worcester, was charged by criminal complaint with possession with intent to distribute methamphetamine. Following an initial appearance before U.S. District Court Chief Magistrate Judge M. Page Kelley, Kristo was detained pending a detention hearing scheduled for June 30, 2021.
According to the charging document, over the course of two months, Kristo allegedly sold significant quantities of counterfeit Adderall pills containing methamphetamine, cocaine and suspected fentanyl to an undercover law enforcement officer.
How to spot fake E 404 pill
Fake E 404 pill does not contain the same ingredients as real E 404 pill. Instead they contain mostly illicit compounds that can cause overdose. Makers of this drug sometimes experience supply issues leading to shortages which is often times exploited by fraudsters who make fake versions of this product and circulate. Makers of generic Adderall, sold as mixed amphetamine salts also have trouble making enough product to meet demand. The shortages often affect extended-release and immediate-release versions of the drugs.
There have been at least two cases in which people received counterfeit versions of the 30-milligram dose of the drug with the wrong active ingredients— ones that treat acute pain, not attention problems. The fake pill is ineffective and may be harmful.
In their latest report on fake online pharmacies that ply their trade in the United States, the National Association of Boards of Pharmacy (NABP) found more than 1,500 new websites that it considers “Not Recommended” and of these, 31% are offering illicit prescription drugs. Studies have shown that poor quality medicines represent a global threat to the public health that can result in treatment ineffectiveness, drug resistance, increased morbidity and mortality rate, economic loss and problems to the healthcare system.
As a consumer, you may not have access to most of the test equipment used by regulatory bodies to verify the identity of a drug product. The following tips will serve as a guide to purchasing genuine E 404 pill and help you avoid fakes;
Visual inspection
Visual inspection as stated by the World Health Organization (WHO) still remains the first step in identifying potential fake drug irrespective of the analytical methods used. This is because such observation serves as a lead to identifying fake products even in the absence of the knowledge of the physical characteristics of a genuine drug product. You are expected to examine carefully both the package and its content before purchase or use.
Visual inspection of the Package
You should:
- Examine the package and check if it appears suspicious or different from what you previously know.
- Check if the security seal has been tampered with by looking for breaks or tears in the sealing tape and seals.
- Look for unusual fonts, font sizes, print colour, and spelling errors.
- Check the legibility of the information on both the primary and secondary packages.
- Check if the batch number, expiry date and manufacturer’s address on the secondary package are the same with that on the primary package.
- Check if the manufacturer’s address is traceable, that is, if it contains the exact location of the company and not just the country address.
- Check if the registration number (FDA number as the case is for products marketed or sold in United States) is properly printed or if it appears to be tampered with.
Visual inspection of the Dosage form
At this stage, you are meant to check for differences in the physical appearance (colour uniformity, size, shape, consistency etc.) of the drug. As stated by WHO, commonly encountered physical defects that should be looked out for in tablets include:
- Excessive powder and/or pieces of tablets at the bottom of the container (from abraded, crushed or broken tablets).
- Cracks or chips in the tablets, swelling, mottling, discoloration, fusion of tablets.
- Appearance of crystal on the walls of the container or on the tablet.
- Hardening or softening, cracking, swelling, mottling or discoloration of capsule shell should also be looked out for.
Source
The source of the drug also determines if you are buying a fake E 404 pill or not. Buying foreign Adderall exposes you to a lot of risk. Filling your prescription in a reputable pharmacy greatly reduces your chances of buying fake drugs while buying from illiterate and unqualified vendors who hawk drugs in buses, motor parks and in the streets increases your chances of buying fake drugs.
Price
This is another way of identifying fake E 404 pill. If the price is far cheaper than what is expected, then you have to think twice. However, this may not always be true especially for some products (fake innovator/generic brands) which may be sold at the same price as the genuine one.
Unexpected side effect
Counterfeit E 404 pill most of the time contains substances other than the appropriate Active Pharmaceutical Ingredient (API). They may contain incorrect substances, improper dosage or hazardous substances like methamphetamine which produce unusual side effects, worsening medical condition after taking it. The medication should be stopped once any of the above is noticed.
According to the Pharmaceutical Research and Manufacturers of America, consumers who purchase medications online should avoid the following: sites that are located outside of the U.S. that do not indicate any physical address; sites that do not have a license by the relevant State Boards of Pharmacy; sites without a licensed pharmacist to answer questions; and websites that do not require a prescription.
Consumers who wish to purchase drugs over the Internet should look for websites that have the Verified Internet Pharmacy Practice Sites seal. These sites, which are created by the National Association of Boards of Pharmacy, are licensed pharmacies selling FDA-approved medications to discourage the sale of counterfeit drugs from illegitimate online sources.
If you have purchased the counterfeit E 404 pill, do not take it or give it to your child. Call the FDA’s Office of Criminal Investigations at 800-551-3989 or go to https://www.fda.gov/OCI.





