India’s High-Stakes Probe into Alleged Bribery Scandal in Toxic Syrup Tests Reaches Climax
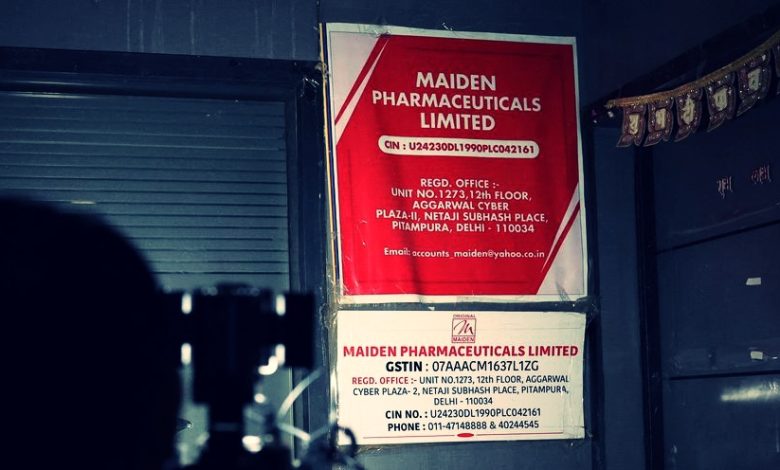
In a significant development, India is reaching the final stages of its investigation into allegations that a state drug regulator accepted a bribe to manipulate samples of cough syrups linked to child deaths in Gambia. The complainant, lawyer Yashpal, accused the drug controller, Manmohan Taneja, of accepting a bribe from Maiden Pharmaceuticals to switch samples before testing.
While the World Health Organization implicated Maiden’s syrups in the deaths of 70 children in Gambia, India’s government contends that tests showed the syrups were not toxic. Maiden Pharmaceuticals has consistently denied any wrongdoing.
Investigation Progress
Gagandeep Singh, joint director at Haryana’s Food and Drugs Administration, confirmed that he is meticulously reviewing Yashpal’s complaint, considering various perspectives, and is on the verge of completing the probe. The government has directed a comprehensive analysis of the complaint, with a consolidated report expected imminently.
Complaint Details and Responses
Yashpal’s complaint alleged that Taneja accepted a bribe of 50 million rupees ($600,687) to manipulate samples before testing at a government laboratory. Taneja dismissed the complaint as fake, and Maiden Pharmaceuticals did not respond to requests for comment.
Government’s Acknowledgment
This marks the first official acknowledgment by a government officer regarding the existence of a detailed investigation into the bribery allegations. The findings will be submitted to Haryana’s FDA Commissioner Ashok Kumar Meena, and any subsequent steps will be determined by superiors.
Witness Account and Investigator’s Remarks
Yashpal, known by a single name, did not appear in person during the investigation but provided statements via email. The investigator noted that Yashpal acknowledged the complaint through email but did not appear in person. The report’s submission will precede any decisions on future actions.
Pharmaceutical Industry Impact
The Maiden Pharmaceuticals case is part of a broader issue involving Indian-made cough syrups linked to child deaths in Gambia, Uzbekistan, and Cameroon, significantly impacting India’s pharmaceutical industry reputation. To address concerns, the government has heightened inspections and made mandatory tests for cough syrups before export.
India’s thorough investigation into these serious allegations underscores the gravity of the situation, emphasizing the need for stringent measures to ensure the safety and reliability of pharmaceutical exports, crucial for maintaining the industry’s international standing.





