How Long Are EpiPens Good For?

Anaphylaxis is a severe, potentially life-threatening allergic reaction. It can occur within seconds or minutes of exposure to something you’re allergic to, such as peanuts or bee stings.
Anaphylaxis causes the immune system to release a flood of chemicals that can cause you to go into shock — blood pressure drops suddenly and the airways narrow, blocking breathing. Signs and symptoms include a rapid, weak pulse; a skin rash; and nausea and vomiting. Common triggers include certain foods, some medications, insect venom, and latex.
What Is an EpiPen?
EpiPen is the brand name of an auto-injectable device that delivers the drug epinephrine. Epinephrine is in a class of medications called alpha- and beta-adrenergic agonists (sympathomimetic agents). It works by relaxing the muscles in the airways and tightening the blood vessels. It is a life-saving medication used when someone is experiencing anaphylaxis.
EpiPen is just one of the brand names of devices known generically as Epinephrine Auto-Injectors. This medication acts on the whole body to block the progression of the allergic response. It constricts the blood vessels, leading to increased blood pressure, and decreased swelling. This allows the muscles around the airways to relax, causing the lungs to open. Epinephrine also prevents the release of more allergic chemicals, which stops the progression of the allergic response.
Epinephrine is the only medication that works on the entire body, multi-system, multi-organ, for anaphylaxis, which is why it is the only drug recommended.
Anaphylaxis requires an injection of epinephrine and a follow-up trip to an emergency room. If you don’t have epinephrine, you need to go to an emergency room immediately. If anaphylaxis isn’t treated right away, it can be fatal.
How Do You Know If You Need Injectable Epinephrine?
First and foremost, if you suspect you have had an allergic reaction to a food or insect sting, you should see a board-certified allergist to evaluate your reaction/symptoms. The allergist will obtain pertinent medical history, perform a physical exam, and recommend diagnostic testing if indicated.
If you already have a diagnosis of food allergy, it is important to see your allergist regularly for possible re-testing and an oral food challenge to determine if you have outgrown some of your allergic triggers. Epinephrine auto-injectors are indicated for patients at risk for anaphylaxis, so in some cases, a prescription may no longer be medically necessary.

How should EpiPen be used?
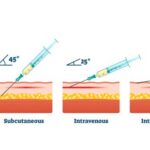
Epinephrine injection comes as a prefilled automatic injection device containing a solution (liquid) and in vials to inject subcutaneously (under the skin) or intramuscularly (into the muscle). It is usually injected as needed at the first sign of a serious allergic reaction. Use epinephrine injection exactly as directed; do not inject it more often or inject more or less of it than prescribed by your doctor.
Ask your doctor or pharmacist to show you and any of your caregivers who could be injecting the medication how to use the prefilled automatic injection device. Training devices are available to practice how to use the automatic injection device during an emergency. Training devices do not contain medication and do not have a needle. Before you use epinephrine injection for the first time, read the patient information that comes with it. This information includes directions for how to use the prefilled automatic injection device. Be sure to ask your pharmacist or doctor if you or your caregivers have any questions about how to inject this medication.
You should inject epinephrine injection as soon as you suspect that you may be experiencing a serious allergic reaction. Signs of a serious allergic reaction include the closing of the airways, wheezing, sneezing, hoarseness, hives, itching, swelling, skin redness, fast heartbeat, weak pulse, anxiety, confusion, stomach pain, losing control of urine or bowel movements, faintness, or loss of consciousness. Talk to your doctor about these symptoms and be sure you understand how to tell when you are having a serious allergic reaction and should inject epinephrine.
Keep your automatic injection device with you or available at all times so that you will be able to inject epinephrine quickly when an allergic reaction begins. Be aware of the expiration date stamped on the device and replace the device when this date passes. Look at the solution in the device from time to time. If the solution is discolored or contains particles, call your doctor to get a new injection device.
Epinephrine injection helps to treat serious allergic reactions but does not take the place of medical treatment. Get emergency medical treatment immediately after you inject epinephrine. Rest quietly while you wait for emergency medical treatment.
Most automatic injection devices contain enough solution for one dose of epinephrine. If your symptoms continue or return after the first injection, your doctor may tell you to use a second dose of epinephrine injection with a new injection device. Be sure that you know how to inject the second dose and how to tell whether you should inject a second dose. Only a healthcare provider should give more than 2 injections for a single allergic episode.
Epinephrine should be injected only in the middle of the outer side of the thigh and can be injected through clothing if necessary in an emergency. If you are injecting epinephrine to a young child who may move during the injection, hold their leg firmly in place and limit the child’s movement before and during the injection. Do not inject epinephrine into the buttocks or any other part of your body such as fingers, hands, feet, or into a vein. Do not put your thumb, fingers, or hand over the needle area of the automatic injection device. If epinephrine is accidentally injected into these areas, get emergency medical treatment immediately.
After you inject a dose of epinephrine injection, some solution will remain in the injection device. This is normal and does not mean that you did not receive the full dose. Do not use the extra liquid; dispose of the remaining liquid and device properly. Take the used device with you to the emergency room or ask your doctor, pharmacist, or healthcare provider how to dispose of used injection devices safely.
How long does an EpiPen last?
EpiPen has a relatively short shelf life due to the instability of epinephrine. EpiPen 0.3mg auto-injector devices have now had their shelf life increased from 20 months to 24 months from the date of manufacture. Expiry dates can be found on the label on the auto-injector device and should not be used after this date. Do not use an expired EpiPen because doing so can trigger unwanted side effects.
EpiPen Safety Issues
FDA recently alerted patients, caregivers, and health care professionals that EpiPen 0.3mg and EpiPen Jr 0.15mg auto-injectors, and the authorized generic versions, may potentially have delayed injection or be prevented from properly injecting due to:
- Device failure from spontaneous activation caused by using sideways force to remove the blue safety release
- Device failure from inadvertent or spontaneous activation due to a raised blue safety release
- Difficulty removing the device from the carrier tube
- User errors
In a letter to health care professionals from Pfizer, the manufacturer of the EpiPen, and Mylan, detailed how these devices may activate prematurely if the blue safety release is removed using a sideway force. For example, a user may try to hold a device with only one hand and try to remove the blue safety release with their thumb in a sideways force. Prior to use, the blue safety release should be removed by pulling straight up with one hand and holding the device with the other hand.
A very limited number of EpiPen devices also may have a blue safety release that is slightly raised. If the blue safety release is raised, the device may activate prematurely, which could potentially delay or prevent emergency treatment when needed.
Additionally, in some cases, EpiPen devices may not slide out of their carrier tube easily, or potentially at all, due to a slight deformation on the rim of the carrier tube. The carrier tube is the immediate package in which the auto-injector is contained. In some cases, the patient or caregiver may not be able to quickly remove the auto-injector from the carrier tube.
The letter also describes specific user errors that can delay or prevent the administration of the intended dose of epinephrine. For example:
- The device will not activate if the blue safety release is in place
- Ensure the needle end (orange end of the device) is in contact with the outer thigh (upper leg) prior to and during activation. The EpiPen device should be administered by swinging and pushing firmly against the outer thigh until it “clicks.” This signals that injection has started.
- Ensure the device is held in place for a minimum of three seconds following activation.
It is important for health care providers, patients, and caregivers to periodically review the EpiPen user instructions and practice using the EpiPen trainer to ensure proper understanding and utilization of the EpiPen auto-injector.
It is vital for lifesaving products to work as designed in an emergency situation, and patients and caregivers should inspect their epinephrine auto-injector prior to needing it to ensure the blue safety release is not raised and that the device can be easily removed from the carrier tube.
Patients should contact Mylan Customer Relations at 800-796-9526 if they find an issue with their auto-injector and to obtain a replacement at no additional cost. Pharmacists should inspect the products before dispensing them to patients to ensure quick access to the auto-injector and should not dispense any product which does not easily slide out of its carrier tube or has a raised blue safety release. As stated on the product label, consumers should always seek emergency medical help right away after using their epinephrine auto-injector.
FDA is aware of adverse event reports associated with EpiPen products. FDA asks health care professionals and consumers to report any adverse reactions or quality problems to the FDA’s MedWatch program:
- Complete and submit the report online at www.fda.gov/medwatch/report.htm.
- Download and complete the form, then submit it via fax at 1-800-FDA-0178.
What are the side effects of EpiPen?
EpiPen may cause side effects. When you get emergency medical treatment after you inject epinephrine, tell your doctor if you are experiencing any of these side effects:
• skin redness, swelling, warmth, or tenderness at the site of injection
• difficulty breathing
• pounding, fast, or irregular heartbeat
• nausea
• vomiting
• sweating
• dizziness
• nervousness, anxiety, or restlessness
• weakness
• pale skin
• headache
• uncontrollable shaking of a part of your body.