Drug-induced Hepatitis
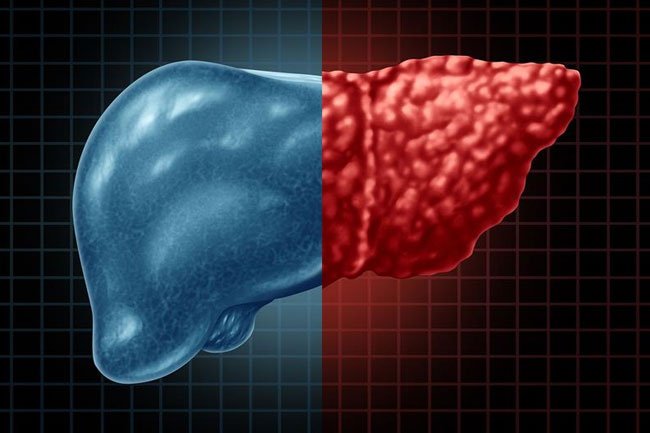
What is drug-induced hepatitis?
Drug-induced hepatitis is a redness and swelling (inflammation) of the liver that is caused by a harmful (toxic) amount of certain medicines. The liver helps to break down certain medicines in your blood. If there is too much medicine in your blood for your liver to break down, your liver can become badly damaged. This can lead to drug-induced hepatitis.
More than 900 drugs, toxins, and herbs have been reported to cause liver injury, and drugs account for 20-40% of all instances of fulminant hepatic failure. Approximately 75% of the idiosyncratic drug reactions result in liver transplantation or death. Drug-induced hepatic injury is the most common reason cited for withdrawal of an approved drug.
What causes drug-induced hepatitis?
Drug-induced hepatitis is rare. It is caused when you have a harmful or toxic amount of some medicines, vitamins, herbal remedies, or food supplements.
In most cases, you may be taking a medicine for several months before it reaches a toxic level and affects your liver. But the disease can also happen if you take too much of some medicines, such as acetaminophen. In this case, it can happen quickly. Other times, it is an allergic reaction.
Many types of medicines may cause drug-induced hepatitis. These include:
• Pain and fever medicines that have acetaminophen
• Aspirin and over-the-counter pain and fever medicines (NSAIDs or nonsteroidal anti-inflammatory medicines)
• Anabolic steroids, man-made medicines that are like the male sex hormone testosterone
• Some medicines used to treat bacterial infections (antibiotics)
• Birth control pills (oral contraceptives)
• Statins, used to lower cholesterol
• Sulfa medicines, a type of antibiotic
• Anti-epileptic medicines
• Herbal medicines, including ephedra, Germander, Pennyroyal, and many others. Keep in mind that not all “natural” or “herbal” supplements are safe. They are also not regulated for safety.
Who is at risk for drug-induced hepatitis?
The risk for drug-induced hepatitis varies with each medicine.
You may be at higher risk for drug-induced hepatitis if you:
• Have liver disease, such as from long-term alcohol use, HIV, or viral hepatitis
• Drink alcohol and take medicines at the same time
• Are older
• Are a woman
• Use long-acting or extended release medicines
• Take multiple medicines that contain acetaminophen. There are many medicines both over-the-counter and prescription with acetaminophen.
• Use herbal supplements
What are the symptoms of drug-induced hepatitis?
The following are the most common symptoms of drug-induced hepatitis. However, each individual may experience symptoms differently.
Symptoms may include:
- Fever
- Rash or itchy red hives on skin
- Joint pain
- Sore muscles
- Flu-like symptoms
- Nausea
- Vomiting
- Decreased appetite
- Sore muscles
- Jaundice – yellowing of the skin and eyes
The symptoms of drug-induced hepatitis may resemble other medical conditions or problems. Always consult your physician for a diagnosis.
How is drug-induced hepatitis diagnosed?
Your healthcare provider will look at your past health and give you a physical exam.
You may have some lab blood tests, including:
- Liver function tests. These check for any redness and swelling (inflammation) or damage to the liver.
- Complete blood count or CBC. Looks at the number and types of cells in your blood.
- Coagulation studies. These tests look at how well the liver makes proteins that cause blood to clot.
- Electrolyte panel. Checks to see if you have too many or too few minerals (electrolyte imbalance) in your blood.
- Other tests to evaluate for liver disease, such as viral hepatitis labs, iron studies, and others.
- Tests for other chemicals in your body.
- Drug screening tests.
Your may also have the following tests:
- Ultrasound. This is used to see your liver and check how blood is flowing through different blood vessels. High-frequency sound waves create images of your internal organs on a computer screen.
- CT scan. This is an imaging test that uses X-rays and a computer to make detailed images of the body. A CT scan shows details of the bones, muscles, fat, and organs.
- MRI. This uses electromagnetic energy to create a picture of the organs.
- Liver biopsy. Small tissue samples are taken from your liver with a needle. These samples are checked under a microscope to find out the amount and type of liver damage you have.
How is drug-induced hepatitis treated?
You must stop taking the medicine that is causing the problem. You must also check your liver closely while it recovers. The liver is often able to heal itself.
In severe cases, you may need to be in the hospital as your liver heals.
In rare situations, the liver fails and you will need a liver transplant.
Some medicines may cause a slight increase in liver enzymes without any symptoms. You may not need to stop using these medicines. Talk with your healthcare provider about the risks and benefits.
What are the complications of drug-induced hepatitis?
If you don’t stop taking the medicine that is causing the problem, your liver will become more damaged. It may not recover. If this happens, you will need a liver transplant.
Key points about drug-induced hepatitis
• Drug-induced hepatitis is a redness and swelling (inflammation) of the liver.
• It is a rare condition caused by harmful (toxic) amounts of certain medicines, vitamins, herbal remedies, or food supplements.
• In most cases, you may be taking a medicine for several months before it reaches a toxic level and affects your liver.
• You may also get the condition if you take too much of some medicines, such as acetaminophen. This can happen quickly.
• You must stop taking the medicine that is causing the disease.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
• Know the reason for your visit and what you want to happen.
• Before your visit, write down questions you want answered.
• Bring someone with you to help you ask questions and remember what your provider tells you.
• At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
• Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
• Ask if your condition can be treated in other ways.
• Know why a test or procedure is recommended and what the results could mean.
• Know what to expect if you do not take the medicine or have the test or procedure.
• If you have a follow-up appointment, write down the date, time, and purpose for that visit.
• Know how you can contact your provider if you have questions.