Blue C1 Pill: Uses, Side Effects, Addiction, Warnings
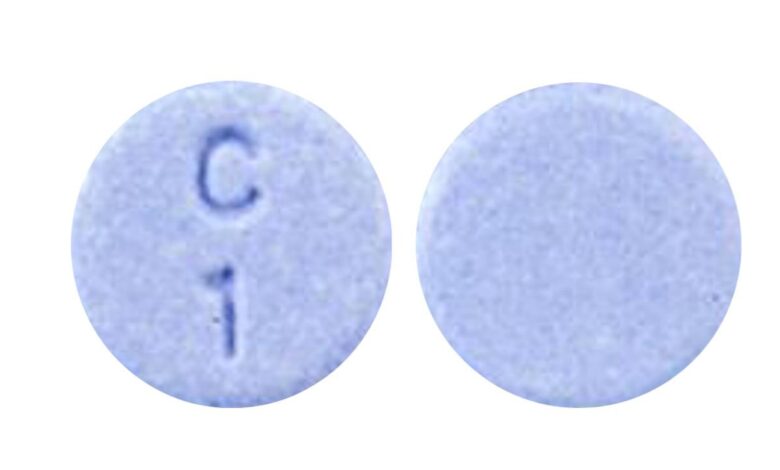
The blue round pill with the imprint C 1 has been identified as Clonazepam 1 mg supplied by Accord Healthcare, Inc.. Clonazepam 1 mg is classified as a Schedule 4 controlled substance under the Controlled Substance Act (CSA). Clonazepam belongs to the class of medications called benzodiazepines. In general, benzodiazepines are used as a sedative or to decrease seizures or anxiety. C 1 pill is used to treat seizure disorders. It helps by slowing the activity of the nerves in the brain (i.e., the central nervous system).
Your doctor may have suggested C 1 pill for conditions other than those listed in this drug information article. If you have not discussed this with your doctor or are not sure why you are taking this medication, speak to your doctor. Do not stop taking this medication without consulting your doctor.
Who should NOT take C 1 pill?
Do not use C 1 pill if you:
• are allergic to clonazepam, or any ingredients of the medication
• have had an allergic reaction to any other benzodiazepine (e.g., lorazepam, diazepam, oxazepam)
• have acute narrow or closed angle glaucoma
• have myasthenia gravis
• have severe breathing problems
• have severe liver disease
• have sleep apnea
C 1 pill may be used by people with open angle glaucoma who are receiving appropriate treatment.
What are the possible side effects of C 1 pill?
The following side effects have been reported by at least 1% of people taking C 1 pill. Many of these side effects can be managed, and some may go away on their own over time.
Contact your doctor if you experience these side effects and they are severe or bothersome. Your pharmacist may be able to advise you on managing side effects.
• clumsiness or unsteadiness
• delayed reaction
• dizziness or lightheadedness
• drowsiness
• increased watering of the mouth
• muscle weakness
• unusual tiredness or weakness
Although most of the side effects listed below don’t happen very often, they could lead to serious problems if you do not seek medical attention.
Check with your doctor as soon as possible if any of the following side effects occur:
• abnormal thinking (disorientation, delusions, or loss of sense of reality)
• anxiety
• behavior changes (e.g., aggressiveness, agitation, unusual excitement, nervousness, or irritability)
• confusion
• convulsions (seizures)
• cough
• hallucinations (hearing or seeing things that aren’t there)
• increased falls
• memory loss of recent events
• nightmares or trouble sleeping
• signs of depression (e.g., poor concentration, changes in weight, changes in sleep, decreased interest in activities, thoughts of suicide)
Stop taking the medication and seek immediate medical attention if any of the following occur:
• signs of a severe allergic reaction (e.g., hives; difficulty breathing; or swelling of the mouth, tongue, lips, or throat)
• thoughts of self-harm, suicide
Some people may experience side effects other than those listed. Check with your doctor if you notice any symptom that worries you while you are taking this medication.
Are there any other precautions or warnings for this medication?
Before you begin taking a medication, be sure to inform your doctor of any medical conditions or allergies you may have, any medications you are taking, whether you are pregnant or breast-feeding, and any other significant facts about your health. These factors may affect how you should take this medication.
Alcohol: People taking this medication should not consume alcohol since doing so can reduce the effectiveness of this medication and increase the risk of side effects. People who have an addiction to alcohol or other drugs should not take C 1 pill except in rare situations under medical supervision.
Breathing: C 1 pill can suppress breathing. This effect on breathing may be more pronounced for people with breathing problems, brain damage, or who are taking other medications that suppress breathing (e.g., codeine, morphine). If you have severe breathing problems, discuss the risks and benefits of taking this medication your doctor.
Coordination problems: If you have a medical condition that affects coordination (e.g., spinal or cerebellar ataxia, discuss with your doctor how this medication may affect your medical condition, how your medical condition may affect the dosing and effectiveness of this medication, and whether any special monitoring is needed.
Dependence and withdrawal: Physical dependence (a need to take regular doses to prevent physical symptoms) has been associated with benzodiazepines such as C 1 pill. Severe withdrawal symptoms may occur if the dose is significantly reduced or suddenly stopped. These symptoms include seizures, irritability, nervousness, sleep problems, agitation, tremors, diarrhea, abdominal cramps, vomiting, memory impairment, headache, muscle pain, extreme anxiety, tension, restlessness, and confusion. Reducing the dose gradually under medical supervision can help prevent or decrease these withdrawal symptoms. Do not suddenly stop taking this medication without talking to your doctor.
Depression: C 1 pill, like other benzodiazepines, has been known to cause mood swings and symptoms of depression. If you have depression or a history of depression, discuss with your doctor how this medication may affect your medical condition, how your medical condition may affect the dosing and effectiveness of this medication, and whether any special monitoring is needed. If you experience symptoms of depression such as poor concentration, changes in weight, changes in sleep, decreased interest in activities, or notice them in a family member who is taking this medication contact your doctor as soon as possible.
Clonazepam is not recommended for use by people with depression or psychosis or who have attempted suicide.
Drowsiness/reduced alertness: Because C 1 pill causes drowsiness and sedation, avoid activities requiring mental alertness, judgment, and physical coordination (such as driving or operating machinery) while taking it. This is particularly true when first taking the medication and until you have established how clonazepam affects you. Alcohol can increase the drowsiness effects and should be avoided.
Grapefruit juice: Avoid drinking grapefruit juice while you are taking this medication as it can increase the levels of clonazepam in your blood.
Kidney function: Decreased kidney function or kidney disease may cause this medication to build up in the body, causing side effects. If you have kidney disease or reduced kidney function, discuss with your doctor how this medication may affect your medical condition, how your medical condition may affect the dosing and effectiveness of this medication, and whether any special monitoring is needed.
Lactose intolerance: Lactose is one of the ingredients in this medication. If you have a hereditary condition that makes you intolerant to lactose, discuss other alternatives with your doctor.
Liver function: If you have liver disease or decreased liver function, discuss with your doctor how this medication may affect your medical condition, how your medical condition may affect the dosing and effectiveness of this medication, and whether any special monitoring is needed. People with severe liver problems should not take this medication.
Memory: This medication may impair recent memory. If you experience this while taking this medication, contact your doctor.
Porphyria: If you have porphyria, discuss with your doctor how this medication may affect your medical condition, how your medical condition may affect the dosing and effectiveness of this medication, and whether any special monitoring is needed.
Seizures: For some people taking this medication, seizures may worsen or a new type of seizure can occur. If you experience worsening seizures or the frequency of your seizures does not decrease while taking this medication, contact your doctor.
Pregnancy: Taking C 1 pill during pregnancy can increase the risk of certain birth defects. This medication should only be used during pregnancy if the benefits outweigh the risks. If you become pregnant while taking this medication, contact your doctor immediately. Do not stop taking this medication suddenly, as this may result in withdrawal symptoms. Discuss the options with your doctor and follow their instructions closely.
Breast-feeding: This medication passes into breast milk. If you are a breast-feeding mother and are taking C 1 pill, it may affect your baby. Talk to your doctor about whether you should continue breast-feeding.
Children: If long-term use of C 1 pill is being considered for a child, discuss with your child’s doctor the benefits and the risks of C 1 pill use. Long-term use may have an effect on your child’s physical and mental development.
Seniors: Seniors may be at increased risk for the sedative and impaired coordination effects of this medication. This can increase the risk of falls and fractures. Seniors may require lower doses of this medication.
What other drugs could interact with this medication?
There may be an interaction between clonazepam and any of the following:
• abiraterone acetate
• alcohol
• antihistamines (e.g,. cetirizine, doxylamine, diphenhydramine, hydroxyzine, loratadine)
• antipsychotics (e.g., chlorpromazine, clozapine, haloperidol, olanzapine, quetiapine, risperidone)
• aprepitant
• azelastine
• “azole” antifungals (e.g., itraconazole, ketoconazole, voriconazole)
• barbiturates (e.g., butalbital, phenobarbital)
• benzodiazepines (e.g., alprazolam, diazepam, lorazepam)
• bicalutamide
• boceprevir
• bosentan
• brimonidine
• buspirone
• calcium channel blockers (e.g., amlodipine, diltiazem, nifedipine, verapamil)
• chloral hydrate
• clonidine
• cobicistat
• conivaptan
• crizotinib
• dabrafenib
• dasatinib
• deferasirox
• dronedarone
• efavirenz
• entacapone
• enzalutamide
• general anesthetics (medications used to put people to sleep before surgery) grapefruit juice
• HIV non-nucleoside reverse transcriptase inhibitors (e.g., delavirdine, efavirenz, etravirine, nevirapine)
• HIV protease inhibitors (e.g., atazanavir, indinavir, ritonavir, saquinavir)
• imatinib
• kava kava
• macrolide antibiotics (e.g., clarithromycin, erythromycin)
• magnesium sulfate
• methadone
• mifepristone
• mirtazapine
• mitotane
• modafinil
• muscle relaxants (e.g., baclofen, cyclobenzaprine, methocarbamol, orphenadrine)
• narcotic-containing medications (e.g., codeine, oxycodone, morphine)
• nabilone
• nefazodone
• norfloxacin
• olopatadine
• pramipexole
• proton pump inhibitors (e.g., lansoprazole, omeprazole)
• rifabutin
• rifampin
• ropinirole
• St. John’s wort
• scopolamine
• seizure medications (e.g., clobazam, carbamazepine, levetiracetam, phenobarbital, phenytoin, primidone, topiramate, valproic acid, zonisamide)
• selective serotonin reuptake inhibitors (SSRIs; e.g., citalopram, duloxetine, fluoxetine, paroxetine, sertraline)
• siltuximab
• simeprevir
• tapentadol
• tetrahydrocannabinol
• thalidomide
• theophyllines (e.g., aminophylline, oxtriphylline, theophylline)
• tocilizumab
• tolcapone
• tramadol
• tricyclic antidepressants (e.g., amitriptyline, clomipramine, desipramine, trimipramine)
• valerian
• zolpidem
• zopiclone
If you are taking any of these medications, speak with your doctor or pharmacist. Depending on your specific circumstances, your doctor may want you to:
• stop taking one of the medications,
• change one of the medications to another,
• change how you are taking one or both of the medications, or
• leave everything as is.
An interaction between two medications does not always mean that you must stop taking one of them. Speak to your doctor about how any drug interactions are being managed or should be managed.
Medications other than those listed above may interact with this medication. Tell your doctor or prescriber about all prescription, over-the-counter (non-prescription), and herbal medications that you are taking. Also tell them about any supplements you take. Since caffeine, the nicotine from cigarettes, or street drugs can affect the action of many medications; you should let your prescriber know if you use them.





