Inflammatory Bowel Disease (IBD) Symptoms That Are Easy to Miss

Inflammatory Bowel Disease (IBD) has a long and evolving history that dates back to ancient times. Early medical texts from ancient civilizations, such as Egypt and Greece, made references to individuals suffering from symptoms resembling IBD, though a clear understanding of the condition was lacking at the time. It wasn’t until the 20th century that significant strides were made in recognizing and defining IBD as a distinct medical entity.
The discovery of Crohn’s disease marked a pivotal moment in the history of IBD. In 1932, three American gastroenterologists – Dr. Burrill B. Crohn, Dr. Leon Ginzburg, and Dr. Gordon D. Oppenheimer – published a seminal paper on “Terminal Ileitis,” later recognized as Crohn’s disease. This groundbreaking work brought IBD to the forefront of medical attention, shedding light on the inflammation of the gastrointestinal tract.
As medical technology advanced, distinguishing between the two major forms of IBD, Crohn’s disease, and ulcerative colitis, became possible. Endoscopy and colonoscopy allowed for direct visualization of the inflamed intestinal tissues, aiding in more accurate diagnosis and differentiation of the diseases. Additionally, research in genetics and immunology revealed the role of genetic predisposition and an overactive immune response in IBD development, leading to more targeted treatment approaches.
In recent years, significant progress has been made in IBD management through the development of biological therapies. These drugs specifically target components of the immune system responsible for the inflammatory response, offering new hope for patients with moderate to severe IBD. Ongoing research continues to explore the complex mechanisms underlying IBD and potential new treatment avenues, aiming to improve the quality of life for those affected by this chronic and challenging condition. In this article, we will explore some of the less obvious IBD symptoms that are easy to miss.
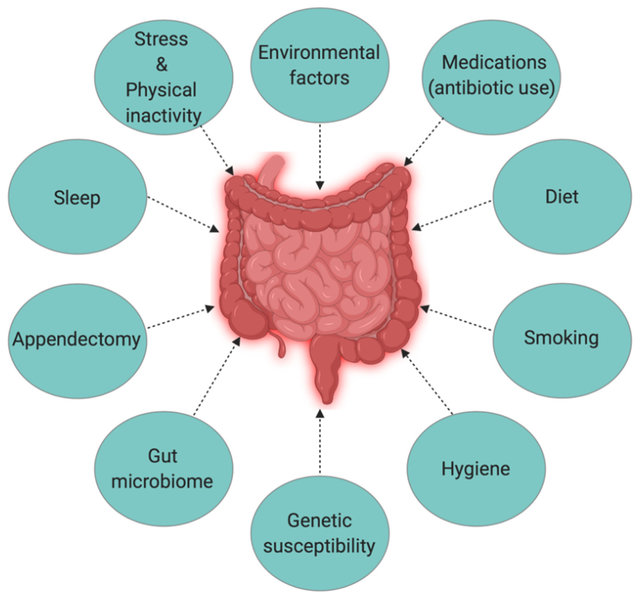
Causes
Inflammatory Bowel Disease (IBD) is a complex condition with multifactorial causes. While the exact etiology remains unclear, several factors contribute to the development of IBD. Some of these causes may lead to subtle symptoms that are easy to miss, delaying the diagnosis and appropriate management. Here are some potential causes of IBD symptoms that can be overlooked:
1. Genetic Predisposition: IBD tends to run in families, indicating a genetic component. Certain gene mutations or variations can increase the likelihood of developing IBD. If there is a family history of IBD, individuals may be more susceptible to the condition, and seemingly minor symptoms could be early indicators of the disease.
2. Dysregulated Immune Response: IBD is considered an autoimmune disorder, where the immune system mistakenly attacks the gastrointestinal tract. The immune system’s overreaction leads to chronic inflammation, which may present with mild, intermittent symptoms that are easily ignored or attributed to other causes.
3. Environmental Triggers: Environmental factors, such as diet, infections, and exposure to certain toxins, may influence the development or exacerbation of IBD. These triggers can be challenging to identify, and their effects on the gastrointestinal system may initially manifest as mild digestive discomfort or irregular bowel movements.
4. Microbiome Imbalance: The gut microbiome plays a crucial role in maintaining gut health and immune regulation. An imbalance in the gut microbiome, known as dysbiosis, is associated with IBD. Subtle changes in the microbiome might result in nonspecific symptoms that are not immediately linked to IBD.
5. Stress and Lifestyle: Chronic stress, poor dietary choices, lack of exercise, and smoking can contribute to gut inflammation and aggravate existing IBD symptoms. These lifestyle factors may not always be seen as connected to gastrointestinal health, leading to missed opportunities for early intervention.
6. Asymptomatic or Mild Flares: IBD symptoms can fluctuate in intensity, with periods of remission and mild flares. During remission or when symptoms are mild, individuals may overlook or dismiss early signs of IBD, attributing them to temporary issues.
7. Extraintestinal Manifestations: IBD can affect other parts of the body beyond the gastrointestinal tract. Symptoms like joint pain, skin rashes, eye irritation, or mouth sores may not immediately raise suspicion for IBD, leading to delayed diagnosis.
Early recognition and timely medical evaluation are essential for diagnosing IBD and initiating appropriate management to improve long-term outcomes and quality of life for individuals affected by this chronic condition.
Inflammatory bowel disease (IBD) Symptoms That Are Easy to Miss
The following are 6 inflammatory bowel disease (IBD) symptoms that are easy to miss:
1. Fatigue and Weakness
Feeling fatigued and weak is a common complaint, but it can be particularly insidious in the context of IBD. Chronic inflammation in the intestines leads to poor nutrient absorption and anemia, which results in persistent tiredness and a lack of energy. Fatigue in IBD can sometimes be attributed to a busy lifestyle or stress, leading to delayed diagnosis. If you notice an unexplained and ongoing feeling of exhaustion, it’s important to consult a healthcare professional for further evaluation.
2. Joint Pain
Joint pain and stiffness are symptoms that are often associated with arthritis or other musculoskeletal disorders. However, in some cases, IBD can manifest with similar joint issues. This condition, known as enteropathic arthritis, occurs due to the immune system’s response to inflammation in the intestines, affecting the joints as well. It can lead to swollen, tender, and painful joints, which may be mistaken for other forms of arthritis.
3. Skin Problems
IBD can also present itself through various skin manifestations. Rashes, sores, or ulcers on the skin might be overlooked as unrelated dermatological conditions. In reality, these skin problems can be a result of the inflammatory response that occurs in IBD. Conditions like pyoderma gangrenosum and erythema nodosum are examples of skin issues associated with IBD, but their connection can be easily missed, leading to delayed diagnosis and management.
4. Eye Irritations
Red, dry, and irritated eyes can be due to many reasons, such as allergies or computer strain. However, in some IBD patients, ocular inflammation can occur as a complication of the disease. Uveitis is the most common eye condition associated with IBD, and it can cause eye pain, sensitivity to light, and blurred vision. If you experience persistent eye discomfort alongside other potential IBD symptoms, it’s essential to bring this to your healthcare provider’s attention.
5. Mouth Sores
Canker sores or ulcers in the mouth are often seen as minor annoyances that will resolve on their own. However, they can also be a sign of IBD. Oral manifestations like aphthous stomatitis can accompany gut inflammation, and if they become recurrent or chronic, it should prompt further investigation.
6. Unexplained Weight Loss
While significant weight loss is an apparent symptom of IBD, it’s often attributed to dieting or other lifestyle changes. Unintentional weight loss can be a crucial indicator of underlying health issues, including IBD. Chronic inflammation in the gastrointestinal tract can interfere with nutrient absorption, leading to a drop in body weight even when eating a seemingly balanced diet.
How is IBD treated?
The treatment of Inflammatory Bowel Disease (IBD), which includes Crohn’s disease and ulcerative colitis, involves the use of various medications to control inflammation, manage symptoms, and maintain remission. The choice of medication depends on the type and severity of IBD and the individual’s response to treatment. Here are some of the commonly used medications for IBD:
1. Aminosalicylates (5-ASAs)
• Examples: Mesalamine, Sulfasalazine, Balsalazide, Olsalazine.
• Used for: Mild to moderate IBD, mainly in ulcerative colitis.
• Mechanism: These drugs reduce inflammation in the intestines and are often the first-line treatment for mild cases.
2. Corticosteroids
• Examples: Prednisone, Prednisolone, Budesonide.
• Used for: Acute flare-ups or severe IBD to rapidly reduce inflammation and control symptoms.
• Mechanism: These potent anti-inflammatory drugs work by suppressing the immune response.
3. Immunomodulators
- Examples: Azathioprine, 6-Mercaptopurine, Methotrexate.
• Used for: Maintenance therapy to reduce inflammation and achieve remission in moderate to severe IBD.
• Mechanism: These medications suppress the overactive immune system to decrease inflammation.
4. Biologics (Anti-TNF Agents)
• Examples: Infliximab, Adalimumab, Certolizumab, Golimumab.
• Used for: Moderate to severe IBD when other treatments have not been effective.
• Mechanism: Biologics target specific proteins involved in the inflammatory process, such as TNF-alpha, to reduce inflammation.
5. Biologics (Anti-Integrins)
• Examples: Vedolizumab, Natalizumab.
• Used for: Moderate to severe IBD, particularly when TNF inhibitors are not suitable.
• Mechanism: These drugs target integrins involved in immune cell movement to the gut, reducing inflammation.
6. Janus Kinase (JAK) Inhibitors
• Example: Tofacitinib.
• Used for: Moderately to severely active ulcerative colitis.
• Mechanism: JAK inhibitors interfere with the signaling pathways involved in inflammation.
7. Antibiotics
• Example: Ciprofloxacin, Metronidazole.
• Used for: Infections or complications associated with IBD, such as fistulas in Crohn’s disease.
• Mechanism: Antibiotics can help manage bacterial overgrowth and infections in the intestines.
8. Pain Medications
• Examples: Acetaminophen, Tramadol.
• Used for: Providing relief from the pain associated with IBD.
• Note: Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and aspirin should be avoided in IBD, as they can worsen inflammation.
It’s essential to remember that each person’s response to medications may vary, and the choice of treatment should be based on the individual’s specific condition and medical history. Treatment plans for IBD often involve a combination of medications, lifestyle changes, and close monitoring by healthcare professionals to optimize symptom management and improve the overall quality of life for patients.
How to reduce the risk of developing IBD
There are certain strategies and lifestyle changes that may help reduce the risk of developing IBD or minimize its severity in individuals at higher risk. Here are some prevention guidelines based on current knowledge:
1. Healthy Diet: Adopting a well-balanced, nutritious diet may play a role in reducing the risk of IBD. Incorporate plenty of fruits, vegetables, whole grains, lean proteins, and healthy fats into your meals. Limit processed foods, excessive sugar, and unhealthy fats, as they may contribute to inflammation and gut dysbiosis.
2. Avoiding Triggers: If you have already been diagnosed with IBD or have a family history of the condition, identify and avoid any triggers that exacerbate symptoms. Common triggers can include certain foods, stress, smoking, or certain medications.
3. Regular Exercise: Engaging in regular physical activity can have a positive impact on overall health, including the gastrointestinal system. Exercise can help regulate bowel movements, reduce inflammation, and boost the immune system.
4. Avoid Smoking: Smoking has been linked to an increased risk of developing Crohn’s disease and can worsen symptoms in individuals with IBD. If you are a smoker, quitting can significantly improve your overall health.
5. Manage Stress: Chronic stress can negatively affect the immune system and exacerbate inflammation. Engage in stress-reducing activities such as yoga, meditation, or spending time in nature to promote relaxation.
6. Hydration: Drinking an adequate amount of water each day is essential for maintaining good digestive health and preventing complications that may arise from dehydration.
7. Antibiotic Use: Avoid unnecessary or excessive use of antibiotics, as it can disrupt the balance of gut bacteria and potentially trigger inflammation.
8. Breastfeeding: Studies suggest that breastfeeding in infancy may offer some protection against the development of IBD later in life.
9. Regular Health Check-ups: If you have a family history of IBD or are experiencing any gastrointestinal symptoms, it’s essential to seek medical attention promptly. Early detection and intervention can lead to better outcomes and management.
It’s important to note that while these preventive measures may help reduce the risk of developing IBD, they are not guaranteed to prevent the condition entirely. IBD is a complex disease with various genetic, environmental, and immunological factors contributing to its development. If you suspect you may have IBD or are at risk, consult a healthcare professional for personalized advice and appropriate monitoring.
Conclusion
Inflammatory Bowel Disease (IBD) is a complex and often challenging condition to diagnose, as its symptoms can overlap with other common ailments. Recognizing the less obvious signs of IBD is essential for early detection and effective management of the disease. If you experience any of the mentioned symptoms persistently, it is crucial to consult a healthcare professional for a thorough evaluation. Timely diagnosis and appropriate treatment can significantly improve the quality of life for individuals living with IBD.





